Introduction
Imagine waking up each morning feeling like your body is fighting against itself. You plan your day, hoping for some relief, but the fatigue sets in like a wave, joint pain makes even simple tasks feel overwhelming, and brain fog clouds your thoughts. For many living with autoimmune diseases, this is a daily reality. Now, consider facing not just one, but multiple autoimmune conditions simultaneously—each adding its own layer of complexity.
Managing polyautoimmunity—where multiple autoimmune diseases coexist—goes beyond addressing individual conditions. It’s about understanding the intricate ways these diseases interact and influence one another, often amplifying symptoms and complicating both diagnosis and treatment. Polyautoimmunity is becoming increasingly recognized as more individuals, like myself, navigate these overlapping conditions. For those with even more severe cases, such as Multiple Autoimmune Syndrome (MAS), where three or more autoimmune diseases occur, the challenges can be even more pronounced.
As someone diagnosed with Hashimoto’s thyroiditis, narcolepsy, and rheumatoid arthritis, I’ve faced these complexities firsthand. This blog post aims to shed light on the nuances of polyautoimmunity and MAS, exploring their causes, distinctions between primary and secondary autoimmune diseases, and strategies for effective management. By sharing my journey and insights, I hope to provide practical guidance and support for those managing similar challenges.
What is Polyautoimmunity?
Polyautoimmunity involves not only the presence of multiple autoimmune diseases but also the complexity and unpredictability of how these conditions interact. When an individual has multiple autoimmune diseases, symptoms often overlap, making it challenging to pinpoint which disease is responsible for specific issues. This overlap can lead to delays in diagnosis, as healthcare professionals work to identify and differentiate each condition accurately.
For instance, up to 25% of individuals with autoimmune thyroid disease may also develop conditions like type 1 diabetes or rheumatoid arthritis.
In my journey, I have experienced the complexities of polyautoimmunity firsthand. I was initially diagnosed with Hashimoto’s thyroiditis in 2015, which came with symptoms of brain fog, weight changes, and sensitivity to cold. Managing this condition was challenging enough, but for years, I also dealt with persistent excessive daytime sleepiness and insomnia. After thorough evaluations, I was finally diagnosed with narcolepsy in 2019. The combination of these conditions was overwhelming, as each brought its own set of symptoms and treatment requirements.
Adding to these challenges, I had been dealing with joint issues that progressively worsened over the years. Initially, I attributed these problems to osteoarthritis. However, when I started to experience symmetrical muscle and joint pain, I realized there might be more to my condition. Seeking medical advice, I underwent further evaluations and was eventually diagnosed with rheumatoid arthritis in 2023. This diagnosis added significant joint pain and stiffness to my daily battles, further complicating my health journey.
The interplay between these diseases has made it challenging to distinguish which symptoms belong to which condition, complicating both diagnosis and treatment. Living with multiple autoimmune diseases has heightened my awareness of the necessity for comprehensive care and self-advocacy. It has also highlighted the critical need for increased awareness and understanding of polyautoimmunity within the autoimmune community. By sharing my experiences, I hope to provide valuable insights and support to others facing similar challenges.
In the next section, we will explore the distinctions between primary and secondary autoimmune diseases. Understanding these categories is essential for accurate diagnosis and effective management of polyautoimmunity and MAS.
Primary vs. Secondary Autoimmune Diseases
Primary Autoimmune Diseases: These are the first autoimmune conditions diagnosed in an individual, typically marking the initial onset of immune system dysfunction. These diseases can vary significantly in their impact and the systems they affect. Examples include rheumatoid arthritis, where the immune system mistakenly targets the synovial joints, causing pain and inflammation, and systemic lupus erythematosus (lupus), which can affect multiple organ systems, such as the skin, kidneys, and cardiovascular system. Primary autoimmune diseases often require immediate intervention to manage inflammation and prevent damage.
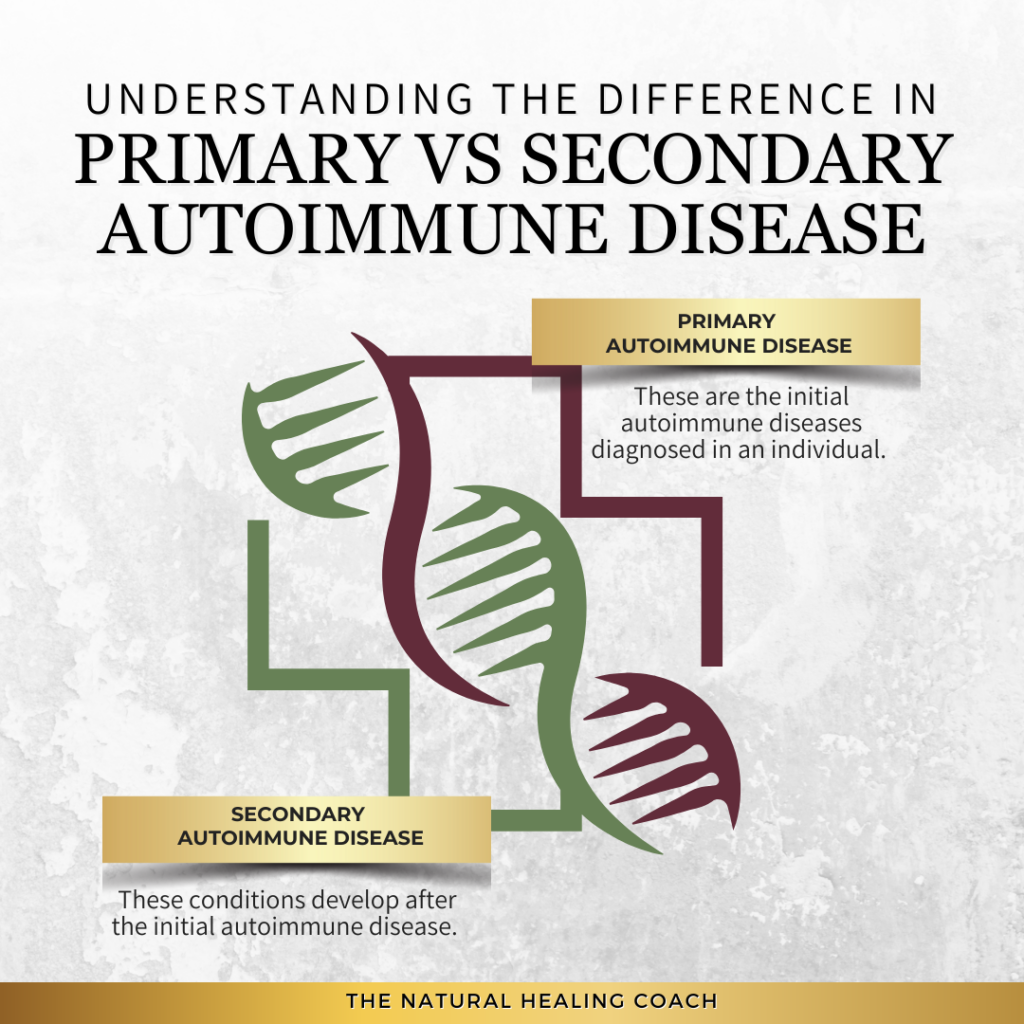
Secondary Autoimmune Diseases: These conditions develop after the initial diagnosis of a primary autoimmune disease. They are often triggered by or associated with the ongoing immune dysregulation from the primary condition. For example, an individual with lupus (the primary disease) may later develop autoimmune thyroiditis (secondary), where the immune system begins to attack the thyroid gland. This development can occur due to shared genetic, environmental, or immunological factors that predispose an individual to additional autoimmune conditions.
Interplay Between Primary and Secondary Diseases: The occurrence of secondary autoimmune diseases is frequently linked to the persistent activation and dysregulation of the immune system seen in the primary disease. Once the immune system is in an overactive state, it may begin to target other tissues and organs, leading to a cascade of immune responses. Over time, this immune dysfunction can spread, resulting in multiple affected systems and creating a complex clinical picture. This progression underscores the importance of comprehensive monitoring and tailored treatment plans to manage and mitigate the risks of secondary autoimmune conditions effectively.
Can a Secondary Autoimmune Disease Be Diagnosed Before a Primary?
It is possible for a secondary autoimmune disease to be diagnosed before the primary one, particularly when the symptoms of the secondary condition are more pronounced or appear earlier. In such cases, the initial autoimmune disease may be subtle or progress more slowly, leading to a delayed diagnosis. For instance, a patient might first seek treatment for symptoms associated with Sjogren’s syndrome, such as dry eyes and mouth, which may prompt an initial diagnosis. However, over time, they may develop additional symptoms that ultimately reveal a primary condition like rheumatoid arthritis.
The complex nature of autoimmune diseases means that symptoms can overlap, making it challenging for healthcare providers to distinguish between conditions without comprehensive evaluation. Clinicians must remain vigilant, considering the possibility of multiple autoimmune conditions even when only one set of symptoms is apparent. A thorough diagnostic process, including detailed medical history, physical examination, blood tests for autoantibodies, and imaging studies, is essential to identify all underlying autoimmune diseases.
Additionally, recognizing that some autoimmune diseases may remain latent or less active while others are more prominent highlights the need for continuous monitoring. Over time, as symptoms evolve or new ones arise, healthcare professionals can adjust their diagnostic approach to better capture the full spectrum of autoimmune involvement. Identifying both primary and secondary autoimmune diseases accurately allows for more targeted and effective treatment, improving long-term outcomes for patients.
Implications of Diagnosing a Secondary Autoimmune Disease Before the Primary
When a secondary autoimmune disease is identified before the primary one, it can complicate diagnosis and management, leading to several important implications:
- Delayed Identification of the Primary Disease: Without recognizing the primary condition, its symptoms may continue to worsen, leading to potential health deterioration and complications that could have been managed earlier.
- Partial Symptom Relief: Initial treatment may focus only on the secondary disease, missing the underlying immune dysfunction associated with the primary condition. This often results in inadequate symptom control, as the root cause remains unaddressed.
- Misaligned Treatment Strategies: Focusing on the secondary disease without addressing the primary condition can result in treatment plans that are not fully effective, as they may overlook broader immune system involvement that impacts both conditions.
- Risk of Overlapping Symptoms Being Misattributed: Overlapping symptoms can make it challenging to distinguish between conditions, potentially leading healthcare providers to misattribute symptoms to the diagnosed secondary disease rather than investigating further.
- Complications in Achieving Comprehensive Care: Without a full understanding of the underlying autoimmune dynamics, healthcare providers may struggle to develop a holistic approach, leading to fragmented care that fails to address the interconnected nature of multiple conditions.
By understanding these implications, both healthcare providers and patients can adopt a more thorough and vigilant approach to managing polyautoimmunity effectively.
Strategies for Effective Management of Polyautoimmunity
Given the complexities associated with polyautoimmunity, especially when secondary autoimmune diseases are diagnosed first, implementing effective management strategies is crucial:
- Comprehensive Diagnostic Evaluations: Conduct thorough medical histories, use advanced diagnostic tools, and screen for multiple autoimmune markers to identify all underlying conditions early.
- Multidisciplinary Care Teams: Collaborate with specialists such as rheumatologists, endocrinologists, and neurologists to create an integrated care plan that addresses the complexities of managing multiple autoimmune diseases.
- Holistic Treatment Plans: Develop individualized treatment strategies that include medication management, lifestyle adjustments, and complementary therapies to address the interconnected nature of symptoms and conditions.
- Regular Monitoring and Adjustments: Schedule consistent follow-up appointments to monitor the progression of each condition and make necessary adjustments to treatment plans based on new symptoms or diagnostic findings.
- Patient Education and Empowerment: Inform patients about the possibility of multiple autoimmune diseases and provide resources for self-management, including dietary guidance, stress management techniques, and symptom tracking tools.
These strategies help ensure that both healthcare providers and patients are equipped to manage polyautoimmunity effectively, improving long-term outcomes and quality of life.
Common Combinations of Autoimmune Diseases
Because polyautoimmunity often involves the coexistence of multiple autoimmune diseases, it often leading to a complex clinical picture. Here are some common combinations of autoimmune diseases seen in individuals with polyautoimmunity:
Examples:
- Rheumatoid Arthritis and Sjögren’s Syndrome: Rheumatoid arthritis primarily affects the joints, causing pain and inflammation. When combined with Sjögren’s syndrome, which affects moisture-producing glands, patients may experience severe dry eyes and mouth in addition to joint symptoms.
- Lupus and Autoimmune Thyroiditis: Lupus is a systemic condition affecting multiple organs, while autoimmune thyroiditis targets the thyroid gland. Individuals with both conditions may have a mix of systemic symptoms such as fatigue and joint pain alongside thyroid-related issues like weight gain or loss, and temperature sensitivity.
- Celiac Disease and Type 1 Diabetes: Celiac disease involves an immune response to gluten, leading to intestinal damage, while type 1 diabetes is characterized by the destruction of insulin-producing cells in the pancreas. This combination can complicate dietary management and blood sugar control.
Implications: Having multiple autoimmune diseases can significantly complicate both diagnosis and treatment. Overlapping symptoms may lead to delayed or missed diagnoses, and managing multiple conditions requires a coordinated approach to treatment. Medications for one disease may interact negatively with treatments for another, necessitating careful management by healthcare providers.
Symptoms of Polyautoimmunity
Shared Symptoms: Many autoimmune diseases share common symptoms, making it challenging to pinpoint the exact cause without comprehensive testing. Common overlapping symptoms include:
- Fatigue: A prevalent symptom in most autoimmune conditions, often leading to severe exhaustion.
- Joint Pain: Common in diseases like rheumatoid arthritis, lupus, and Sjögren’s syndrome.
- Inflammation: Generalized inflammation can affect various parts of the body, contributing to pain and swelling.
Unique Symptoms: Despite the overlap, certain symptoms are unique to specific disease combinations:
- Rheumatoid Arthritis and Sjögren’s Syndrome: Severe joint pain combined with pronounced dry eyes and dry mouth.
- Lupus and Autoimmune Thyroiditis: Malar rash (butterfly rash) on the face along with thyroid-related symptoms such as unexplained weight changes.
- Celiac Disease and Type 1 Diabetes: Gastrointestinal symptoms like diarrhea and bloating, alongside frequent urination and excessive thirst.
Impact on Daily Life: Polyautoimmunity can severely impact the quality of life and daily functioning. Patients may struggle with:
- Physical Limitations: Chronic pain, fatigue, and joint stiffness can make everyday tasks difficult.
- Dietary Restrictions: Conditions like celiac disease and type 1 diabetes require strict dietary management, adding to the complexity of meal planning and eating out.
- Emotional and Mental Health: The burden of managing multiple chronic illnesses can lead to stress, anxiety, and depression.
By understanding the complexities and nuances of polyautoimmunity, patients and healthcare providers can work towards more effective management strategies, improving overall quality of life.
Diagnosing Polyautoimmunity
Diagnostic Challenges: Diagnosing multiple autoimmune diseases can be incredibly challenging due to overlapping symptoms and the complexity of distinguishing between different conditions. Symptoms such as fatigue, joint pain, and inflammation are common to many autoimmune diseases, making it difficult to identify the specific conditions present without thorough and precise testing.
Diagnostic Tools:
- Blood Tests: These are crucial for detecting specific markers of autoimmune activity. Tests such as antinuclear antibody (ANA), rheumatoid factor (RF), and other specific antibodies can help identify particular autoimmune diseases.
- Imaging Studies: Techniques like MRI and ultrasound can reveal inflammation and damage in joints, organs, and tissues, providing visual evidence to support a diagnosis.
- Biopsies: Taking a small sample of tissue from affected areas (e.g., skin, liver, intestines) can help confirm an autoimmune disease by identifying characteristic patterns of inflammation and damage under a microscope.
Comprehensive Evaluation: A thorough evaluation by a healthcare professional is essential for diagnosing polyautoimmunity. This includes taking a detailed medical history, conducting a comprehensive symptom assessment, and performing appropriate diagnostic tests. Collaboration among specialists, such as rheumatologists, endocrinologists, and gastroenterologists, is often necessary to achieve an accurate diagnosis and effective treatment plan.
Polyautoimmunity Treatment and Management
Integrated Approach: Managing polyautoimmunity requires a comprehensive treatment plan that addresses all underlying autoimmune diseases. This approach ensures that the treatment for one condition does not negatively impact the management of another and helps in achieving overall health and well-being.
Medications:
- Immunosuppressants: These drugs help control the immune system’s overactivity and reduce inflammation, preventing further tissue damage.
- Biologics: Targeted therapies that interfere with specific pathways in the immune system, helping to control severe or refractory autoimmune conditions.
- Anti-inflammatory Drugs: Medications such as NSAIDs (nonsteroidal anti-inflammatory drugs) help reduce pain and inflammation associated with autoimmune diseases.
Lifestyle Adjustments:
- Diet: The Autoimmune Protocol (AIP) is designed to reduce inflammation and support gut health by focusing on nutrient-dense foods and eliminating potential dietary triggers.
- Exercise and Movement: Regular physical activity tailored to the individual’s abilities can help maintain mobility, reduce inflammation, and improve overall well-being.
- Stress Management: Techniques such as mindfulness, meditation, and relaxation exercises can help manage stress, which can exacerbate autoimmune symptoms.
- Sleep Hygiene: Prioritizing quality sleep is essential for immune system function and overall health. Establishing a regular sleep schedule and creating a restful sleep environment can improve sleep quality.
Support Systems:
Building a strong support network is crucial for managing polyautoimmunity. This includes:
- Support Groups: Joining groups, either in-person or online, provides a sense of community and shared experiences, offering emotional and practical support.
- Counseling: Professional counseling can help manage the emotional and psychological impact of living with multiple chronic illnesses.
- Healthcare Team: Developing a collaborative relationship with a team of healthcare providers ensures comprehensive care and better management of all autoimmune conditions.
By adopting an integrated and holistic approach to treatment and management, individuals with polyautoimmunity can achieve better control of their symptoms, improve their quality of life, and prevent further progression of their conditions.
Final Thoughts
Living with polyautoimmunity is undoubtedly challenging, but understanding and addressing these complexities can greatly improve your quality of life. It’s essential to recognize symptoms early and seek appropriate medical guidance, as early intervention allows for a more comprehensive approach to treatment. This may include a combination of medication, lifestyle modifications, and support systems that work together to manage multiple autoimmune conditions effectively.
Empowering yourself through education and self-advocacy is key. Staying informed about your conditions and available treatment options enables you to make proactive and confident health decisions. Connecting with others who share similar experiences—whether through support groups, online communities, or advocacy efforts—provides both emotional and practical support, reinforcing that you’re not alone on this journey.
Managing polyautoimmunity is not just about alleviating symptoms; it’s about nurturing your overall well-being through a holistic approach. Incorporating strategies like the Autoimmune Protocol (AIP), prioritizing rest, and fostering a supportive healthcare team are critical steps to enhancing your health. Embrace these resources and don’t hesitate to seek help from healthcare professionals and community networks that specialize in autoimmune conditions.
If you’re navigating a diagnosis, supporting a loved one, or simply seeking to learn more, education and awareness are crucial. Stay informed with trusted resources like the Autoimmune Association, the National Institutes of Health (NIH), or the National Institute of Allergy and Infectious Diseases (NIAID). These organizations provide comprehensive information on autoimmune conditions, research, and management strategies.
- Autoimmune Association: https://autoimmune.org
- National Institutes of Health (NIH) on Autoimmune Diseases: https://www.niehs.nih.gov/health/topics/conditions/autoimmune/index.cfm
- Mayo Clinic on Autoimmune Diseases: https://www.mayoclinic.org/diseases-conditions/autoimmune-disease/symptoms-causes/syc-20350647
- National Institute of Allergy and Infectious Diseases (NIAID): https://www.niaid.nih.gov/diseases-conditions/autoimmune-diseases
- Autoimmune Protocol (AIP) Diet Resources: https://www.autoimmunewellness.com
Taking an active role in your health means advocating for yourself and working closely with healthcare providers to develop a personalized plan. Consider participating in research studies or clinical trials to contribute to the advancement of autoimmune disease understanding.
For those looking for more personalized support, I offer comprehensive coaching services through the Autoimmune Protocol (AIP). As a certified AIP coach, I provide guidance to help you implement strategies that work for your unique health needs. You can learn more about my services and how I can support you on your journey at https://naturalhealing.coach/autoimmune-protocol. Together, we can work towards achieving optimal health and well-being.
Call to Action
If you found this information helpful and want to learn more about managing autoimmune conditions and staying active, we invite you to engage with our community. Join the conversation, share your experiences, and connect with others who are on the same journey towards better health.
Stay Informed and Connected
- Engage on Social Media: Follow us on your favorite social media platforms for daily tips, inspiration, and community support. We regularly share practical advice, uplifting stories, and the latest research on exercising with autoimmune conditions. Join the conversation and be part of a supportive community.
Subscribe to Our Newsletter
- Exclusive Insights: Get in-depth articles and updates on the latest research in autoimmune health directly to your inbox.
- Health Tips: Receive practical tips and strategies for managing your condition and improving your overall well-being.
- Stay Updated: Be the first to know about new blog posts, upcoming events, and other valuable resources.
Join the Discussion
- Leave a Comment: We’d love to hear your thoughts and experiences. Share your insights in the comments below and connect with others who are on the same journey. Your comments help build a supportive community where everyone can learn and grow together.
Together, we can take proactive steps towards better health and well-being, even with autoimmune disease.
If you are looking for more tips and support, join me over on my group page, The Village – A Natural HEALing Community, to get tons of information and tips to help you take your HEALTHY EATING and ACTIVE LIVING to the next level.
REFERENCES:
- Anaya, J. M. et al. (2014). “The kaleidoscope of autoimmunity: Multiple autoimmune syndromes.” Autoimmunity Reviews.
- Pimentel-Quiroz, V. R., et al. (2021). “Polyautoimmunity and Systemic Lupus Erythematosus.” Rheumatology International.
- Tobón, G. J., et al. (2022). “Frequency of Polyautoimmunity in Patients With Autoimmune Diseases.” Journal of Clinical Rheumatology.
- Paloma Health. (n.d.). “Hashimoto’s and Polyautoimmunity: Multiple Autoimmune Syndrome.”
MORE RELATED POSTS:








+leave a comment . . .