Introduction
Ever felt too tired to move, let alone exercise? You’re not alone. Imagine this: It’s 5 PM, and after a long, grueling day of work, all you want to do is collapse on the couch. The thought of lacing up your running shoes feels impossible, even though you know deep down that a bit of exercise would likely make you feel better in the long run. This scenario is all too common.
Studies show that up to 45% of adults experience regular fatigue, significantly impacting their ability to stay active and maintain a healthy lifestyle. #fatigue #exercise #healcoach Share on XFatigue doesn’t just hit us physically; it can also weigh heavily on our minds. Picture this: You’ve planned a post-work jog all day, but as the time approaches, your body feels like it’s carrying the weight of the world, and your mind is a foggy mess. You’re not just battling tired muscles—you’re fighting against a mental barrier as well. This dual struggle is something many of us face, and it can make the idea of exercising feel like an insurmountable challenge.
In this blog, we will explore practical strategies to manage exercise exhaustion and stay active. We’ll delve into the differences between mental and physical fatigue, helping you understand how each type uniquely affects your ability to maintain a fitness routine. Additionally, we’ll identify other factors that contribute to fatigue, with a special focus on autoimmune disease and how they compound the challenge.
Whether your fatigue stems from physical exertion, mental stress, or underlying health conditions, we’ll provide you with six effective tips to overcome these obstacles. From adjusting your exercise routine to incorporating mind-body practices, these strategies are designed to empower you to overcome fatigue and maintain a healthy, active lifestyle. So, let’s embark on this journey together, finding ways to move forward even when our energy is low.
Understanding Fatigue
Definition and Types of Fatigue
Fatigue is a pervasive sense of tiredness or exhaustion that can significantly impact daily functioning and quality of life. It can manifest in different forms, primarily as mental fatigue and physical fatigue.
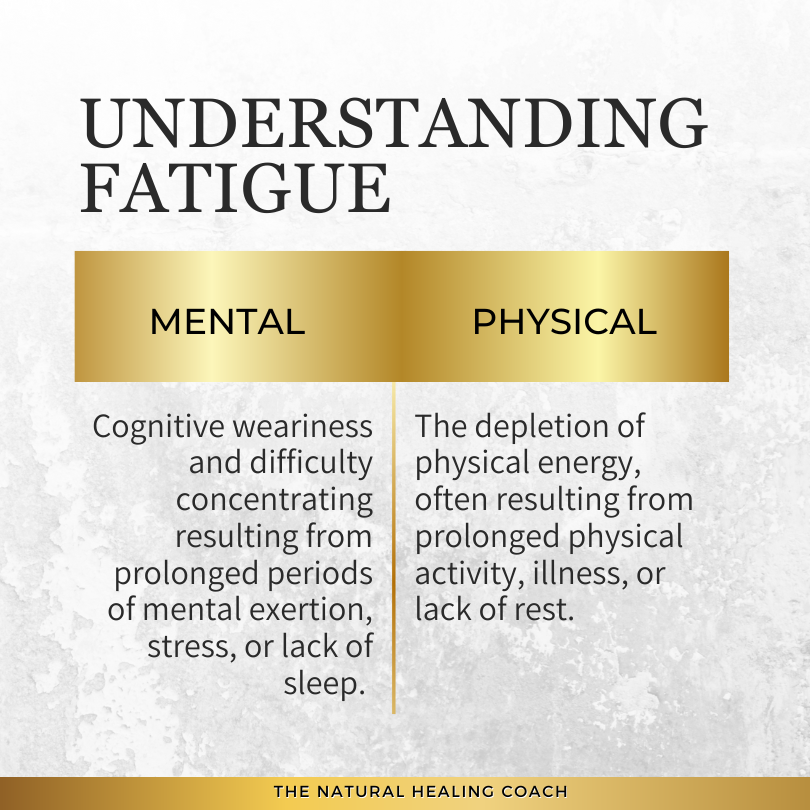
- Mental Fatigue Mental fatigue is characterized by cognitive weariness and difficulty concentrating. It often results from prolonged periods of mental exertion, stress, or lack of sleep. Mental fatigue can make it challenging to perform tasks that require sustained attention and mental effort.
- Physical Fatigue Physical fatigue, on the other hand, refers to the depletion of physical energy, often resulting from prolonged physical activity, illness, or lack of rest. Physical fatigue can make even simple tasks like walking up stairs or carrying groceries feel daunting.
Biological Causes of Mental vs. Physical Fatigue
BIOLOGICAL CAUSES OF FATIGUE
Fatigue is a complex symptom with various underlying biological causes. Understanding these causes is essential for developing effective strategies to manage and alleviate fatigue. Below, we explore the primary biological factors contributing to both mental and physical fatigue.
Biological Causes of Mental Fatigue:
- Neurotransmitter Imbalance: Mental fatigue can be linked to imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine, which affect mood, focus, and energy levels.
- Brain Inflammation: Chronic inflammation in the brain can lead to cognitive fatigue, often seen in conditions like depression and chronic stress.
- Sleep Deprivation: Lack of restorative sleep disrupts normal brain function, leading to impaired cognitive performance and increased mental fatigue.
- Hormonal Changes: Fluctuations in hormones, such as cortisol and thyroid hormones, can impact brain function and contribute to mental fatigue.
- Chronic Inflammation: Chronic inflammation, often found in autoimmune diseases and other chronic conditions, can lead to sustained mental fatigue due to its effect on the body’s energy resources and cognitive functions.
- Chronic Illness: Conditions such as chronic fatigue syndrome and anemia can affect overall energy levels, impacting mental stamina and cognitive functions.
- Mitochondrial Dysfunction: Issues with mitochondria, the energy-producing structures in cells, can lead to reduced energy production, impacting cognitive function.
Biological Causes of Physical Fatigue:
- Muscle Glycogen Depletion: Prolonged physical activity can deplete glycogen stores in muscles, leading to physical exhaustion.
- Lactic Acid Buildup: Intense exercise can cause a buildup of lactic acid in muscles, resulting in soreness and fatigue.
- Mitochondrial Dysfunction: Issues with mitochondria, the energy-producing structures in cells, can lead to reduced energy production and increased physical fatigue.
- Chronic Inflammation: Systemic inflammation can affect muscle performance and recovery, contributing to ongoing physical fatigue, often seen in autoimmune diseases and other chronic conditions.
- Chronic Illness: Conditions such as anemia, hypothyroidism, and chronic fatigue syndrome directly affect energy levels and physical stamina.
- Sleep Deprivation: Prevents muscle recovery, contributing to physical exhaustion.
- Hormonal Changes: Affect overall energy balance, influencing physical energy levels.
Recognizing the distinct biological causes of mental and physical fatigue is crucial for developing targeted and effective management strategies. By addressing the specific factors contributing to each type of fatigue, individuals can implement tailored approaches to enhance their energy levels and overall quality of life. Whether through medical treatment, lifestyle adjustments, or supportive therapies, understanding and tackling the root causes of fatigue is a critical step towards achieving better health and well-being.
To provide a clearer picture of these causes, here is a detailed table outlining the biological causes of mental and physical fatigue and their overlap:
Table 1. Biological Causes of Mental vs. Physical Fatigue
| Biological Cause | Mental Fatigue | Physical Fatigue | Overlap |
|---|---|---|---|
| Neurotransmitter Imbalance | Linked to imbalances in serotonin, dopamine, and norepinephrine, affecting mood, focus, and energy levels | Not typically a direct cause | No |
| Brain Inflammation | Chronic inflammation in the brain, often seen in depression and chronic stress, leading to cognitive fatigue | Not typically a direct cause | No |
| Sleep Deprivation | Disrupts brain function, leading to impaired cognitive performance and increased mental fatigue | Prevents muscle recovery, contributing to physical exhaustion | Yes |
| Hormonal Changes | Fluctuations in cortisol and thyroid hormones impacting brain function and contributing to mental fatigue | Affect overall energy balance, influencing both cognitive and physical energy levels | Yes |
| Muscle Glycogen Depletion | Not typically a direct cause | Prolonged physical activity depletes glycogen stores in muscles, leading to exhaustion | No |
| Lactic Acid Buildup | Not typically a direct cause | Intense exercise causes a buildup of lactic acid in muscles, resulting in soreness and fatigue | No |
| Mitochondrial Dysfunction | Reduces overall energy production, affecting cognitive function | Issues with mitochondria lead to reduced energy production and increased physical fatigue | Yes |
| Chronic Illness | Conditions like chronic fatigue syndrome and anemia affecting overall energy levels | Conditions such as anemia, hypothyroidism, and chronic fatigue syndrome directly affect physical stamina | Yes, particularly with systemic inflammation |
| Chronic Inflammation | Contributes to cognitive fatigue, particularly in conditions like depression and autoimmune diseases | Systemic inflammation can affect muscle performance and recovery | Yes, particularly with systemic inflammation |
Mental vs Physical Fatigue Symptoms
Understanding the distinct differences between mental and physical fatigue, particularly their symptoms, is crucial for effectively managing and mitigating their impact on your daily life and exercise routine. Each type of fatigue manifests differently, affects your body and mind in unique ways, and requires specific strategies for management and recovery.
SYMPTOMS OF FATIGUE
Mental Fatigue Symptoms:
- Difficulty Concentrating: Mental fatigue makes it hard to focus on tasks, leading to decreased productivity and effectiveness.
- Short-term Memory Problems: Forgetfulness and trouble remembering recent events or information are common with mental fatigue.
- Reduced Problem-Solving Ability: Cognitive processes slow down, making it challenging to think clearly and solve problems efficiently.
- Feeling Overwhelmed or Mentally Exhausted: A constant sense of mental drain, even after activities that are not physically demanding.
- Increased Irritability and Mood Swings: Emotional regulation becomes difficult, resulting in irritability and frequent mood changes.
Physical Fatigue Symptoms:
- Muscle Weakness: Physical fatigue often results in a lack of strength, making it hard to perform physical tasks.
- Decreased Physical Performance: Overall physical capabilities diminish, affecting endurance and stamina.
- Slow Recovery from Physical Activity: The body takes longer to recover after exercise or physical exertion.
- Persistent Tiredness, Even After Rest: Despite rest, there is a lingering sense of exhaustion.
- Reduced Stamina and Endurance: The ability to sustain prolonged physical activity decreases significantly.
By recognizing these symptoms and understanding the underlying causes of mental and physical fatigue, you can develop more effective strategies for managing them. Whether through targeted medical treatments, lifestyle changes, or supportive therapies, addressing the specific symptoms and causes of fatigue is essential for maintaining overall health and well-being.
HOW EACH AFFECTS EXERCISE
Understanding how mental and physical fatigue impact exercise is essential for developing effective strategies to maintain a fitness routine despite feeling exhausted. Each type of fatigue presents unique challenges that can affect your motivation, performance, and overall safety during workouts.
Mental Fatigue and Exercise:
- Reduced Motivation: Mental fatigue can severely impact your desire to exercise. The mental burden makes starting and maintaining a workout regimen challenging.
- Poor Focus: Lack of concentration can lead to poor exercise form, increasing the risk of injury.
- Decreased Cognitive Performance: Activities requiring mental coordination, like complex movements in sports or exercise routines, become more difficult.
Physical Fatigue and Exercise:
- Decreased Physical Capacity: Physical fatigue directly reduces your ability to perform physical activities, resulting in shorter and less intense workouts.
- Increased Risk of Injury: Weakened muscles and slow recovery times heighten the risk of injury during physical activity.
- Lowered Endurance: Sustaining exercise over a long period becomes difficult, leading to shorter exercise sessions and reduced overall fitness.
Recognizing the distinct ways in which mental and physical fatigue affect exercise is crucial for managing your fitness routine effectively. By understanding these impacts, you can tailor your exercise strategies to accommodate your energy levels and minimize the risk of injury. Whether it involves modifying your workout intensity, incorporating more rest, or focusing on mental health practices, addressing both types of fatigue can help you maintain a consistent and safe exercise regimen.
IMPORTANCE OF KNOWING THE DIFFERENCES
In this section, we touched on the biological factors, symptoms, and impacts on exercise associated with both mental and physical fatigue. To reiterate, understanding these differences is crucial for effectively managing your overall health and maintaining an active lifestyle. Here’s why knowing these distinctions is so important:
By recognizing and addressing the specific symptoms and causes of mental and physical fatigue discussed earlier, you can implement effective strategies to maintain an active lifestyle and enhance your overall health and well-being. Next, we will delve into the associative factors that contribute to fatigue, providing further insights to help you manage it more effectively.
Associative Factors Contributing to Exercise Exhaustion
Fatigue can stem from a variety of sources, beyond just the biological factors we discussed earlier. These sources, known as associative factors, encompass lifestyle choices, environmental influences, and other external conditions that can contribute to feelings of exhaustion. Understanding these associative factors is key to managing and mitigating their impact on your energy levels and overall well-being. Here are some of the primary associative factors that can lead to fatigue:
A. Sleep Deprivation
One of the most common causes of fatigue is inadequate sleep. Sleep is essential for the body to recover and repair itself. When you don’t get enough quality sleep, your body doesn’t have the opportunity to restore energy levels, leading to persistent tiredness and decreased physical and mental performance. Chronic sleep deprivation can also lead to more severe health issues, including weakened immune function and an increased risk of chronic conditions.
B. Poor Nutrition
What you eat plays a significant role in your energy levels. A diet lacking essential nutrients can lead to fatigue. Consuming high-sugar and high-fat foods can cause energy spikes and crashes, while insufficient intake of vitamins, minerals, and macronutrients can leave you feeling drained. Proper nutrition is crucial for maintaining steady energy levels throughout the day.
C. Stress and Anxiety
Chronic stress and anxiety can be major contributors to fatigue. When you’re stressed, your body is in a constant state of alertness, which can be physically and mentally exhausting. Stress can also interfere with sleep, further exacerbating fatigue. Managing stress through techniques such as mindfulness, meditation, and regular physical activity can help reduce its impact on your energy levels.
Prolonged stress can lead to adrenal fatigue, where the adrenal glands become overworked and less effective at producing hormones like cortisol. This can result in chronic tiredness, difficulty waking up in the morning, and increased effort needed for everyday tasks. Addressing adrenal fatigue involves stress reduction, a balanced diet, adequate sleep, and gentle exercise.
D. Chronic Illnesses and Conditions
Various chronic illnesses and conditions can cause or contribute to fatigue. These include conditions like anemia, diabetes, heart disease, and more. Among these, autoimmune diseases are particularly notable for their impact on fatigue.
- Autoimmune Diseases Autoimmune diseases, such as rheumatoid arthritis, lupus, and multiple sclerosis, often come with a significant fatigue component. This type of fatigue is more than just feeling tired; it’s a pervasive exhaustion that doesn’t improve with rest. Managing autoimmune-related fatigue requires a comprehensive approach, including medical treatment, lifestyle adjustments, and sometimes specific exercise strategies to help maintain energy levels.
E. Lifestyle Factors
Your daily habits and lifestyle choices can also significantly affect your energy levels.
- Sedentary Behavior Leading a sedentary lifestyle can contribute to fatigue. Lack of physical activity can cause your body to become deconditioned, making everyday activities feel more exhausting. Regular exercise helps boost energy levels by improving cardiovascular health and overall fitness.
- Overtraining Conversely, overtraining or excessive physical activity without adequate rest can lead to fatigue. When you push your body too hard without allowing time for recovery, you can experience burnout and chronic tiredness. Balancing exercise with sufficient rest and recovery is crucial to preventing fatigue from overtraining.
F. Dehydration
Even mild dehydration can lead to significant drops in energy levels and physical performance. Water is essential for various bodily functions, including temperature regulation, joint lubrication, and nutrient transportation. Ensuring adequate hydration throughout the day, especially during and after exercise, can help maintain energy levels and prevent fatigue.
G. Medication Side Effects
Many common medications, including antihistamines, blood pressure medications, and antidepressants, list fatigue as a potential side effect. If you suspect your medication is contributing to your fatigue, consult with your healthcare provider to discuss possible alternatives or adjustments.
H. Poor Work-Life Balance
An imbalanced lifestyle, where work or personal responsibilities dominate at the expense of relaxation and recreation, can lead to chronic fatigue. Ensuring a healthy work-life balance that includes time for leisure, hobbies, and social interactions can help mitigate fatigue.
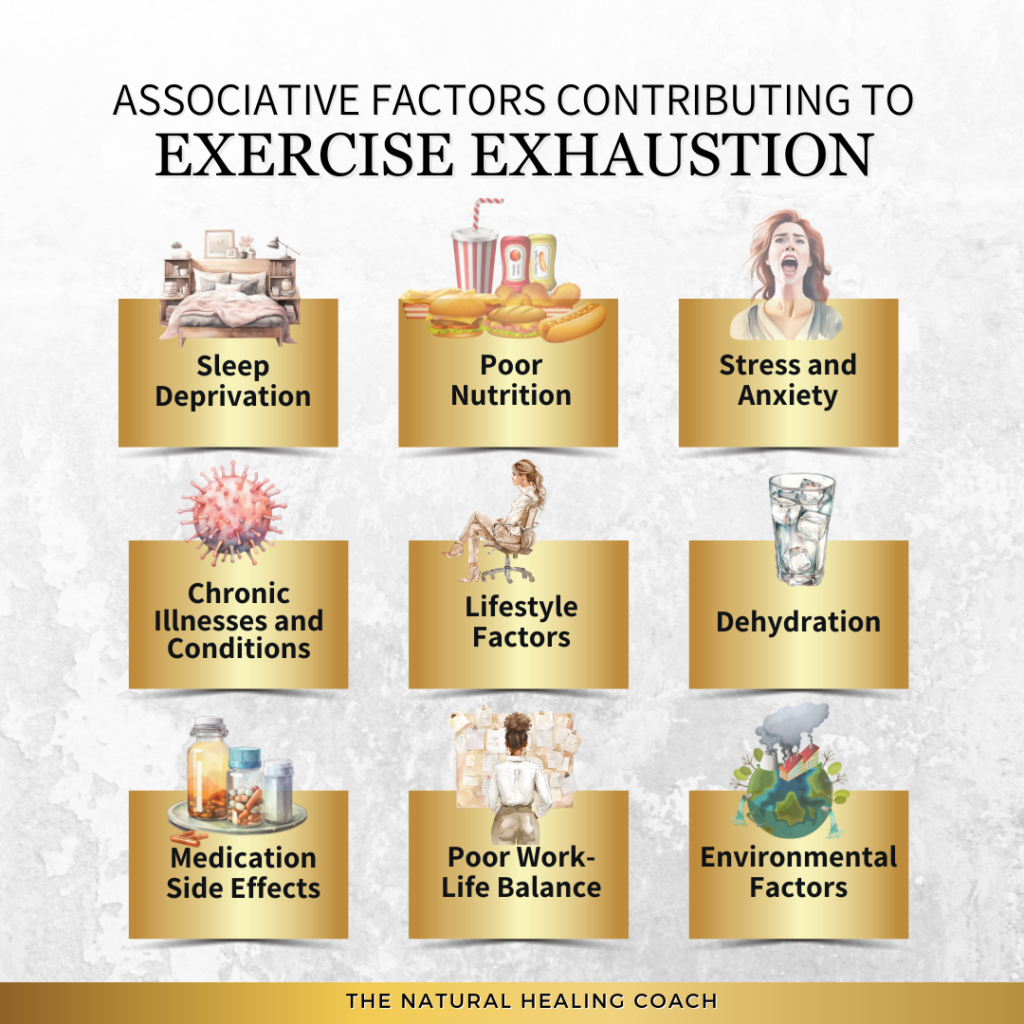
I. Environmental Factors
Factors such as noise pollution, poor air quality, and inadequate lighting can contribute to both mental and physical fatigue. Creating a comfortable, quiet, and well-ventilated environment can improve overall energy levels and reduce feelings of fatigue.
Understanding these associative factors can help you identify potential causes of your fatigue and take steps to address them. By improving sleep, nutrition, stress management, hydration, and balancing physical activity, you can reduce fatigue and enhance your overall well-being.
Managing Exercise Exhaustion: 6 Practical Tips to Stay Active and Fight
Managing fatigue while trying to maintain an exercise routine can be challenging, but with the right strategies, you can stay active and benefit from regular physical activity. Here are some immediate, actionable tips to help you exercise despite feeling fatigued, offering practical advice for integrating exercise into your daily life:
Pay close attention to how your body feels and recognize the signs that you need to rest. Ignoring fatigue can lead to injury and burnout.
- Tips:
- Monitor Your Energy Levels: Keep a daily journal to track how you feel before and after exercise. This can help you identify patterns and adjust your routine accordingly.
- Avoid Overexertion: If you feel unusually tired, opt for lighter activities or take a rest day. It’s better to skip one workout than to risk injury.
- Respect Pain Signals: Pain is a sign that something is wrong. If you experience pain during exercise, stop immediately and consult a healthcare professional if necessary.
Modify your workout routine to suit your energy levels and reduce the risk of overexertion.
Low-Intensity Workouts Opt for exercises that are less demanding on your body.
- Tips:
- Walking: A brisk walk can be as effective as a run without the same level of exertion.
- Swimming: Provides a full-body workout while being gentle on the joints.
- Stretching: Keeps your muscles flexible and can be done anytime, even when you’re feeling fatigued.
Shorter Exercise Sessions Break your workouts into shorter, more manageable sessions throughout the day.
- Tips:
- Mini Workouts: Try 10-15 minute sessions of activity spread throughout the day.
- Interval Training: Alternate between short bursts of activity and rest to keep your workouts effective but less taxing.
- Flexibility in Scheduling: Be flexible with your workout times. If you’re tired in the morning, try exercising later in the day when you might feel more energetic.
Proper hydration and nutrition are crucial for maintaining energy levels.
- Tips:
- Hydrate Regularly: Drink water before, during, and after workouts. Aim for at least 8 glasses a day, more if you are active.
- Balanced Diet: Ensure your meals include a mix of carbohydrates, proteins, and healthy fats to sustain energy levels.
- Pre-Workout Snacks: Eat a light snack 30-60 minutes before exercising, such as a banana or a handful of nuts, to fuel your workout.
Adequate rest and recovery are essential for preventing fatigue and improving performance.
Importance of Sleep Sleep is critical for muscle recovery and overall health.
- Tips:
- Consistent Sleep Schedule: Go to bed and wake up at the same time every day to regulate your internal clock.
- Sleep Environment: Create a restful sleep environment by keeping your bedroom cool, dark, and quiet.
- Limit Stimulants: Avoid caffeine and electronics before bed to improve sleep quality.
Rest Days Incorporate regular rest days into your exercise routine.
- Tips:
- Active Recovery: Engage in low-intensity activities like walking or yoga on rest days to keep your body moving without overexertion.
- Listen to Your Body: If you feel exhausted, take an extra rest day. Rest is just as important as exercise in your fitness journey.
- Massage and Stretching: Use rest days to stretch or get a massage to aid muscle recovery.
Mind-body practices can help manage fatigue by reducing stress and promoting relaxation.
Yoga Yoga combines physical movement with breath control and meditation.
- Tips:
- Gentle Yoga: Choose gentle or restorative yoga classes that focus on stretching and relaxation.
- Breathing Exercises: Incorporate deep breathing techniques to enhance relaxation and reduce stress.
- Consistency: Practice yoga regularly, even if it’s just a few minutes a day, to reap the benefits.
Meditation Meditation helps clear the mind and reduce stress.
- Tips:
- Daily Practice: Aim for at least 5-10 minutes of meditation daily to build a habit.
- Guided Meditation: Use apps or online videos for guided meditation sessions.
- Mindfulness: Incorporate mindfulness techniques throughout the day to stay present and reduce anxiety.
Staying motivated can be challenging when you’re fatigued, but setting goals and tracking progress can help.
Set Realistic Goals Start with small, achievable goals to build confidence and momentum.
- Tips:
- SMART Goals: Set Specific, Measurable, Achievable, Relevant, and Time-bound goals.
- Celebrate Milestones: Reward yourself for reaching milestones, no matter how small.
- Visual Reminders: Use visual reminders like sticky notes or vision boards to keep your goals in sight.
Track Your Progress Monitoring your progress can boost motivation and highlight improvements.
- Tips:
- Fitness Apps: Use fitness apps to track your workouts, steps, and overall activity.
- Journal: Keep a fitness journal to note how you feel before and after exercise and any achievements.
- Photos: Take before and after photos to visually see your progress over time.
By implementing these tips and tricks, you can manage fatigue and maintain an active lifestyle. Remember, it’s essential to listen to your body and adjust your routine as needed to ensure you stay healthy and energized.
Special Considerations for Autoimmune Diseases
Managing autoimmune diseases fatigue involves specific strategies and considerations due to the unique nature of these conditions. This section provides an overview to help navigate exercise and wellness with autoimmune-related fatigue. Here’s how to better manage fatigue and maintain an active lifestyle despite the challenges posed by autoimmune diseases.
Understanding Autoimmune-Related Fatigue
Autoimmune-related fatigue is a profound and persistent exhaustion that goes beyond ordinary tiredness. It can be unpredictable, varying in intensity and duration, and often doesn’t improve with rest alone. This type of fatigue is a common symptom in many autoimmune diseases, such as rheumatoid arthritis, lupus, and multiple sclerosis. Understanding this fatigue as a legitimate and challenging aspect of living with an autoimmune condition is crucial for effective management.
Autoimmune Disease Specific Fatigue: Impact and Reasons
Although fatigue is a common and often debilitating symptom in many autoimmune diseases, certain autoimmune conditions tend to cause more significant fatigue than others due to their specific pathophysiology and the body systems they affect. Here are some autoimmune diseases where fatigue is particularly prominent and the reasons why:
Table 2. Autoimmune Disease Specific Fatigue
| Autoimmune Disease | Impact | Reasons |
|---|---|---|
| Systemic Lupus Erythematosus | High | Systemic inflammation – Organ involvement – Anemia – Medication side effects |
| Multiple Sclerosis | High | Nervous system damage – Heat sensitivity – Sleep disorders – Medication side effects |
| Rheumatoid Arthritis | High | Chronic pain and inflammation – Cytokine production – Poor sleep quality – Comorbid conditions |
| Sjogren’s Syndrome | High | Systemic inflammation – Dryness symptoms – Neurological involvement – Associated fibromyalgia |
| Hashimoto’s Thyroiditis | Moderate to High | Hypothyroidism – Metabolic slowing – Depression |
| Inflammatory Bowel Disease | Moderate to High | Nutrient malabsorption – Chronic inflammation – Anemia – Medication side effects |
| Myasthenia Gravis | Moderate to High | Muscle weakness – Neuromuscular dysfunction – Medication side effects |
| Type 1 Diabetes | Moderate | Blood sugar fluctuations – Insulin management – Comorbid conditions |
| Celiac Disease | Moderate | Nutrient deficiencies – Immune response – Associated conditions |
Understanding which autoimmune diseases have a higher impact on fatigue and the reasons behind it can help patients and healthcare providers tailor management strategies more effectively. Addressing the specific causes of fatigue in these conditions, whether through medical treatment, lifestyle adjustments, or supportive therapies, is crucial for improving quality of life.
Co-Morbidities of Autoimmune Diseases
Autoimmune diseases often occur alongside other chronic conditions, known as co-morbidities. These additional health issues can compound the challenges of managing autoimmune diseases and contribute to overall fatigue. Recognizing and treating these co-morbidities is essential for comprehensive care. Here are some common co-morbidities associated with autoimmune disease:
- Cardiovascular Disease: Individuals with autoimmune diseases are at higher risk for heart disease due to chronic inflammation.
- Osteoporosis: Autoimmune conditions can lead to decreased bone density, increasing the risk of fractures.
- Lung Disease: Autoimmune diseases can lead to pulmonary complications such as interstitial lung disease.
- Kidney Disease: Lupus, for instance, often affects the kidneys, leading to lupus nephritis.
- Mental Health Issues: Depression and anxiety are common co-morbidities that can exacerbate the challenges of managing autoimmune diseases.
- Tips:
- Holistic Approach: Adopt a holistic approach to manage both the autoimmune disease and its co-morbidities effectively.
- Regular Monitoring: Regular check-ups and monitoring of co-morbid conditions can help manage symptoms and prevent complications.
- Collaborative Care: Work with a team of healthcare providers, including specialists, to address all aspects of your health.
Conditions Commonly Confused with Autoimmune Disease
While autoimmune diseases can be a primary cause of fatigue, it’s essential to consider other conditions that may be confused with or occur alongside autoimmune disease due to similar symptoms. Identifying and addressing these conditions can significantly impact energy levels and treatment approaches. Here are some common conditions to consider:
- Chronic Fatigue Syndrome: Often presents with severe fatigue similar to autoimmune conditions.
- Lyme Disease: Can result in autoimmunity and share symptoms like fatigue and joint pain.
- Fibromyalgia: Causes widespread pain and chronic fatigue, frequently overlapping with autoimmune conditions.
- Alzheimer’s or Parkinson’s Disease: These neurodegenerative diseases can sometimes be mistaken for autoimmune conditions due to overlapping symptoms.
- Irritable Bowel Syndrome (IBS): Commonly co-exists with autoimmune diseases, affecting gut health and energy levels.
- Nutrient Deficiency (like Anemia): Reduces the oxygen-carrying capacity of the blood, leading to fatigue, weakness, and shortness of breath.
- Mental Disorders (Depression, Anxiety, Bipolar Disorder): Common among those with autoimmune diseases, contributing to persistent fatigue and decreased motivation.
- Sleep Apnea: Interrupts breathing during sleep, causing daytime fatigue.
- Chronic Infection: Can trigger autoimmunity and share symptoms such as fatigue and pain.
- Migraines: Can be associated with autoimmune conditions and contribute to fatigue.
- Tips:
- Comprehensive Health Check: Ensure you receive a thorough medical evaluation to identify any other underlying conditions that may be contributing to your fatigue.
- Integrated Care: Work with your healthcare provider to develop a comprehensive treatment plan that addresses all potential causes of fatigue, not just the autoimmune disease.
Addressing Hormone and Gut Health Connections
Hormonal imbalances and gut health issues are often interconnected with autoimmune disease and can significantly contribute to fatigue. Understanding and addressing these connections can help manage fatigue more effectively.
HORMONAL IMBALANCES
Imbalances in thyroid hormones, cortisol, and sex hormones can exacerbate fatigue.
- Tips:
- Regular Testing: Work with your healthcare provider to regularly monitor hormone levels.
- Hormone Therapy: Discuss potential hormone therapy or other treatments to address imbalances.
- Lifestyle Adjustments: Implement lifestyle changes such as stress management, balanced nutrition, and adequate sleep to support hormonal health.
GUT HEALTH
The gut plays a crucial role in overall health, including the regulation of immune function and energy levels. Gut dysbiosis and inflammation are common in autoimmune conditions and can contribute to fatigue.
- Tips:
- Probiotics and Prebiotics: Incorporate probiotics and prebiotics into your diet to support a healthy gut microbiome.
- Anti-Inflammatory Diet: Follow an anti-inflammatory diet to reduce gut inflammation and improve digestion.
- Hydration: Ensure adequate hydration to support digestive health and overall well-being.
The Chronic Illness Fitness Journey
Embarking on a fitness journey while managing a chronic illness requires tailored strategies that align with your body’s needs. For those with chronic illnesses, integrating exercise into your routine requires a long-term, sustainable approach to manage and reduce fatigue effectively. Here’s a structured method to help manage and reduce exercise fatigue over the long term:
- Awareness/Acceptance: Recognize and accept that chronic illness often includes fatigue. Understanding the role of exercise in managing symptoms helps set realistic expectations and prepares individuals mentally to incorporate physical activity as a strategy to combat fatigue.
- Consultation: Ensure the exercise plan is safe and effective by consulting healthcare providers. Medical professionals can recommend specific activities that are known to boost energy levels and manage fatigue, tailoring the plan to individual health needs.
- Customization: Personalize the fitness plan to fit one’s abilities and limitations. This ensures that the exercise routine is manageable and not overly taxing, preventing overexertion which can worsen fatigue. Customization allows for the inclusion of energy-boosting activities such as gentle yoga or stretching.
- Gradual Initiation: Start slowly and gradually increase intensity. This helps the body adapt without causing a significant increase in fatigue, building stamina and energy levels over time.
- Monitoring/Feedback: Keep track of how different exercises affect energy levels. Regular monitoring helps identify which activities are most beneficial for reducing fatigue and allows for adjustments based on the body’s response, preventing overexertion.
- Adaptation: Be flexible with the fitness plan, allowing for adjustments on days when fatigue is higher. This prevents pushing the body too hard and allows for lighter activities that still promote energy, like slow walking or tai chi.
- Consistency: Establish a regular exercise routine to help the body become more efficient and resilient over time, leading to improved energy levels and reduced fatigue. Consistent exercise also aids in better sleep, which directly impacts fatigue.
- Progress/Adjustment: Gradually increase the intensity and duration of workouts to build overall endurance, making daily activities less tiring. Adjustments ensure that progress is made without triggering excessive fatigue.
- Support/Community: Having a support system provides motivation and encouragement, making it easier to stick to the exercise routine. Sharing experiences with others facing similar challenges can offer practical tips for managing fatigue.
- Setbacks/Recovery: Recognize that setbacks are part of the journey and develop strategies for gentle movement during flare-ups to maintain some level of activity, preventing fatigue from worsening.
- Sustainability/Maintenance: Ensure the exercise routine is sustainable long-term, making fitness a regular part of life. Balancing exercise with proper rest and nutrition supports overall health and reduces chronic fatigue.
- Education/Empowerment: Educate yourself about managing fatigue through exercise and understand your body
By integrating immediate practical tips with a comprehensive, long-term approach like the Chronic Illness Fitness Journey, individuals with autoimmune diseases can effectively manage and reduce exercise-related fatigue. This balanced strategy ensures that exercise becomes a sustainable part of life, contributing to overall health and well-being. Remember, it’s essential to be patient and compassionate with yourself, recognizing that managing fatigue is a journey that requires continuous adjustment and support. By understanding your body’s needs and working closely with healthcare providers, you can achieve a more active and fulfilling lifestyle despite the challenges of autoimmune-related fatigue.
When to Avoid Exercise
While regular physical activity is generally beneficial, there are specific instances where it may be wiser to refrain from exercising, particularly for those with autoimmune diseases. Recognizing these situations can help prevent exacerbating symptoms and promote recovery. Here are some scenarios where skipping your workout might be the best choice:
GENERAL SITUATIONS TO AVOID EXERCISE
Acute Illness or Infection:
- Fever: Exercising with a fever can increase your body’s internal temperature and make you feel worse.
- Flu or Severe Cold: Your body needs energy to fight off infection, so rest is crucial.
- Infectious Diseases: Conditions like strep throat or mononucleosis require rest and can be exacerbated by physical exertion.
Severe Flare-ups of Chronic Conditions:
- Asthma Attacks: Exercise can exacerbate breathing difficulties during an asthma flare-up.
- Other Chronic Illness Flare-ups: Conditions like heart disease or diabetes may require rest during severe episodes.
Injury:
- Acute Injuries: Injuries such as sprains, strains, or fractures need time to heal. Exercising too soon can delay recovery and worsen the injury.
- Chronic Pain Exacerbation: If chronic pain conditions like fibromyalgia significantly worsen, rest might be necessary.
Post-Surgery or Medical Procedures:
- Recent Surgery: Follow your doctor’s recommendations on when it’s safe to resume physical activity.
- Medical Procedures: After procedures like biopsies or endoscopies, rest is crucial for recovery.
Severe Fatigue or Exhaustion:
- Overtraining Syndrome: Continuous overtraining without adequate rest can lead to chronic fatigue, decreased performance, and increased risk of injury.
- Extreme Physical or Mental Exhaustion: When your body or mind is exceptionally fatigued, rest can help restore energy levels more effectively than exercise.
Additional Considerations for Autoimmune Diseases
For individuals with autoimmune diseases, the decision to exercise can be particularly complex. Here are some specific considerations:
Flare-ups
- Symptom Severity: During mild to moderate flare-ups, gentle exercises like stretching or yoga might be beneficial, but severe symptoms often require rest.
- Listen to Your Body: Pay close attention to your body’s signals. If exercise worsens symptoms, it’s best to stop and rest.
Medication Effects
- Side Effects: Some medications used to treat autoimmune diseases can cause side effects like fatigue, dizziness, or muscle weakness, making exercise difficult.
- Adjustments: Your healthcare provider might need to adjust your exercise plan based on your medication regimen.
Immune System Considerations
- Immunosuppressants: These medications can increase the risk of infections, so avoid crowded places like gyms during high-risk periods.
- Vaccinations and Illnesses: Be cautious with exercise if you’ve recently had vaccinations or if there’s a high risk of catching a contagious illness.
Understanding when to avoid exercise is a vital aspect of managing fatigue and maintaining an effective fitness regimen, especially for those with autoimmune diseases or other chronic conditions. Recognizing when rest and recovery should take precedence can help prevent worsening symptoms, promote healing, and maintain overall well-being. Always consult with healthcare professionals to tailor your activity level to your unique health needs, ensuring you strike the right balance between staying active and allowing your body the rest it needs.
This concept ties directly into the Chronic Illness Fitness Journey, which emphasizes a balanced approach to fitness. Immediate steps to manage exercise fatigue are essential, but for those with chronic illnesses, developing a long-term, sustainable fitness plan is crucial. By incorporating periods of rest and recovery, individuals can maintain an active lifestyle that supports their overall health and well-being without exacerbating their condition. Understanding when to avoid exercise is a key part of this journey, ensuring that fitness routines are safe, effective, and adaptable to changing health needs.
Final Thoughts
Reflecting on the pervasive impact of fatigue in autoimmune diseases, I am reminded of my own journey navigating the complexities of autoimmune-related fatigue. The relentless exhaustion can often feel like an insurmountable barrier, but understanding the specific causes and tailoring management strategies can make a significant difference. It is crucial to acknowledge that fatigue is a legitimate and challenging aspect of living with an autoimmune condition, deserving of compassion and targeted approaches.
To those reading this who are grappling with fatigue, know that you are not alone. Managing fatigue requires patience, persistence, and a willingness to explore different strategies until you find what works best for you. Take small steps, listen to your body, and celebrate even the smallest victories. Remember, progress is progress, no matter how slow it may seem.
The broader implications of effectively managing fatigue extend beyond just improving daily functioning. Addressing fatigue can enhance overall quality of life, enabling you to engage more fully in activities you enjoy and maintain better mental and physical health. It can also foster a deeper understanding of your body’s needs and how to meet them, empowering you to take control of your health journey.
I encourage you to continue exploring the topic of autoimmune-related fatigue. Delve deeper into understanding your specific condition, experiment with different management strategies, and seek support from healthcare providers and communities. The more knowledge you gain, the better equipped you will be to navigate your health challenges and advocate for yourself.
Looking to the future, I envision a world where those with autoimmune diseases have access to comprehensive, personalized care that addresses all facets of their condition, including fatigue. Through continued research, education, and advocacy, we can work towards a future where fatigue is no longer a debilitating aspect of autoimmune diseases but a manageable symptom that individuals can effectively navigate. Let us move forward with hope and determination, knowing that each step taken brings us closer to a brighter, healthier future.
Call to Action
If you found this information helpful and want to learn more about managing autoimmune conditions and staying active, we invite you to engage with our community. Join the conversation, share your experiences, and connect with others who are on the same journey towards better health.
Stay Informed and Connected
- Engage on Social Media: Follow us on your favorite social media platforms for daily tips, inspiration, and community support. We regularly share practical advice, uplifting stories, and the latest research on exercising with autoimmune conditions. Join the conversation and be part of a supportive community.
Subscribe to Our Newsletter
- Exclusive Insights: Get in-depth articles and updates on the latest research in autoimmune health directly to your inbox.
- Health Tips: Receive practical tips and strategies for managing your condition and improving your overall well-being.
- Stay Updated: Be the first to know about new blog posts, upcoming events, and other valuable resources.
Join the Discussion
- Leave a Comment: We’d love to hear your thoughts and experiences. Share your insights in the comments below and connect with others who are on the same journey. Your comments help build a supportive community where everyone can learn and grow together.
Together, we can take proactive steps towards better health and well-being, even with autoimmune disease.
If you are looking for more tips and support, join me over on my group page, The Village – A Natural HEALing Community, to get tons of information and tips to help you take your HEALTHY EATING and ACTIVE LIVING to the next level.
REFERENCES:
- Mayo Clinic. “Fatigue: Symptoms & Causes.”
- American Psychological Association. “Stress Effects on the Body.”
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. “Autoimmune Diseases.”
- Healthline. “What Causes Fatigue?” Available at
- Sleep Foundation. “Sleep Deprivation and Deficiency.”
- American Council on Exercise. “Everything You Need to Know About Exercise and Fatigue.”
- Verywell Fit. “Low-Intensity Workouts.”
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. “Autoimmune Diseases.”
- National Institutes of Health. “Fatigue, Sleep, and Autoimmune and Related Disorders.”
MORE RELATED POSTS:









+leave a comment . . .