Introduction
We’ve all experienced it at some point—a stubbed toe, a scraped knee, or a twisted ankle. One minute you’re going about your day, and the next, you’re wincing in pain as your body reacts to the injury. Almost immediately, the affected area becomes red, swollen, and warm to the touch. This response, while uncomfortable, is a clear sign that your body is hard at work, initiating a process called inflammation to heal the damage.
Inflammation is a natural and essential part of our body’s defense mechanism. When you get hurt or infected, your immune system kicks into action, sending white blood cells to the affected area to fend off harmful invaders and repair damaged tissue. This acute inflammatory response is generally a good thing—it’s our body’s way of protecting us and ensuring we recover from injuries and illnesses.
However, inflammation isn’t always beneficial. When it lingers or occurs without a clear reason, it can become chronic and contribute to a range of health problems, from autoimmune diseases to heart disease. Understanding the nuances of inflammation—what triggers it, how it helps, and when it becomes harmful—is crucial for maintaining overall health and preventing chronic conditions.
In this blog post, we will delve into the complexities of inflammation, exploring the good, the bad, and the often misunderstood aspects of this vital bodily response. By gaining a clearer understanding of inflammation, we can better manage our health and take proactive steps to support our well-being.
What is Inflammation?
Inflammation is the body’s natural response to harmful stimuli, such as pathogens, damaged cells, or irritants. Its primary purpose is to eliminate the cause of cell injury, clear out damaged cells, and initiate the healing process. This complex biological process is crucial for maintaining health and combating various threats to the body.
Recognizing the cardinal signs of inflammation helps in identifying and addressing the underlying causes effectively. #healcoach #inflammtion #autoimmunedisease #chronicillness Share on XThese signs are the body’s way of signaling that something is wrong and needs attention.
There are five cardinal signs of inflammation that indicate the body’s response to injury or infection:
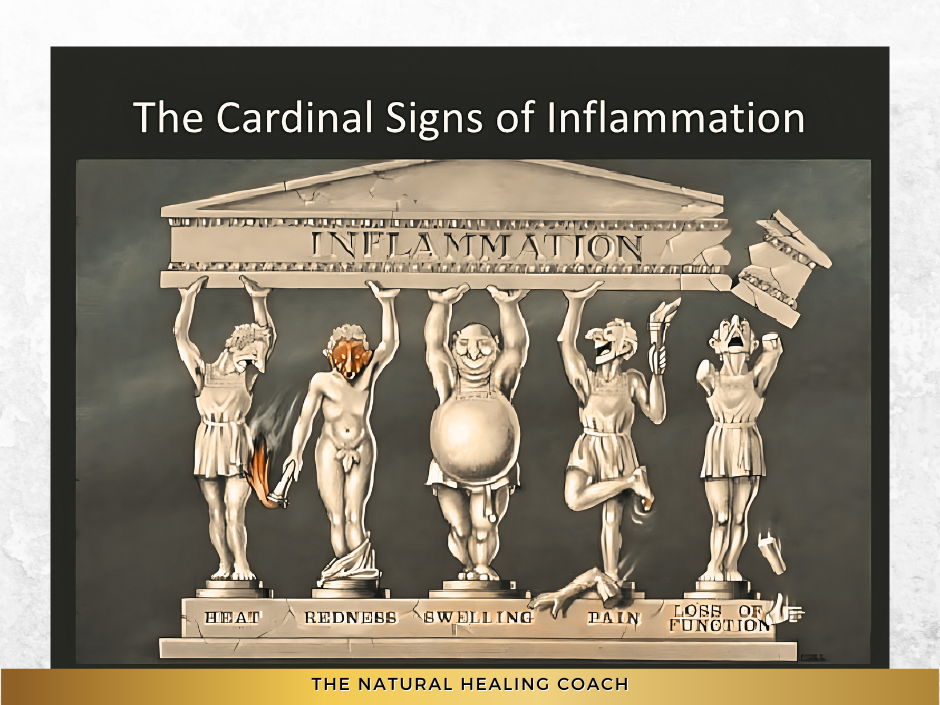
- Heat : The area feels warm due to the increased blood flow.
- Redness: Caused by increased blood flow to the affected area.
- Swelling: Fluid accumulates in the tissues as a result of increased permeability of blood vessels.
- Pain: Inflammatory mediators stimulate nerve endings, causing pain.
- Loss of Function: Swelling and pain can lead to a temporary loss of function in the affected area.
Understanding these signs can help in early detection and proper management of inflammation, ensuring timely medical intervention and effective treatment. However, not all inflammation is the same. It can be broadly categorized into two types: acute and chronic. Recognizing the difference between these types is essential for understanding how inflammation can affect our health in both positive and negative ways.
Explanation of Acute vs. Chronic Inflammation
Acute Inflammation: Acute inflammation is a short-term, immediate response to injury or infection. It manifests as redness, heat, swelling, pain, and sometimes loss of function. This response is typically beneficial as it helps to isolate and eliminate harmful stimuli, prevent further damage, and initiate the healing process. Examples include the redness and swelling around a cut or the pain and heat from a sprained ankle.
Chronic Inflammation: Chronic inflammation, on the other hand, is a prolonged inflammatory response that can last for months or even years. It may result from persistent infections, long-term exposure to irritants, or autoimmune conditions where the immune system mistakenly attacks healthy tissues. Chronic inflammation can lead to tissue damage and is associated with various diseases, such as rheumatoid arthritis, cardiovascular disease, and inflammatory bowel disease.
Table 1: Comparison of Acute and Chronic Inflammation
| Type | Duration | Symptoms | Purpose | Outcome |
|---|---|---|---|---|
| Acute Inflammation | Short-term, immediate response | Redness, heat, swelling, pain, and loss of function | Isolates and eliminates harmful stimuli, initiates healing | Typically resolves once the threat is neutralized |
| Chronic Inflammation | Long-term, persistent response | Can be subtle but persistent, including fatigue, pain, and general malaise | Often misguided, as it occurs even without immediate threats | Can cause tissue damage and contribute to chronic diseases |
The Inflammatory Process
When the body detects harmful stimuli, such as pathogens or damaged cells, it triggers an inflammatory response to protect and heal itself. The inflammatory process can be broken down into several key steps:
Understanding the inflammatory process is crucial for recognizing its dual role in health and disease. While inflammation is essential for defending the body and promoting healing, it must be carefully regulated to prevent chronic inflammation and associated health problems.
The Good, the Bad, and the Misunderstood Aspects of Inflammatory Responses
Inflammation often gets a bad rap, but it’s important to remember that not all inflammation is harmful. In fact, acute inflammation—the body’s immediate and short-term response to injury or infection—is essential for our health. This type of inflammation plays a crucial role in defending the body against pathogens and initiating the healing process. When inflammation functions as it should, it acts as a protector and healer, ensuring that we recover quickly and efficiently from various threats. Let’s explore the beneficial aspects of acute inflammation and understand why it is so vital to our well-being.
The Beneficial Aspects of Acute Inflammation
Healing and Defense: Inflammation is a vital part of the body’s defense mechanism and plays a crucial role in healing. It is the body’s immediate response to injury or infection, designed to protect us from further harm and initiate the healing process.
Fighting Infections: When harmful pathogens like bacteria, viruses, or fungi invade the body, the immune system’s first line of defense is inflammation. The inflammatory response quickly mobilizes white blood cells, specifically neutrophils and macrophages, to the site of infection. These immune cells engulf and destroy the invading microorganisms, preventing them from spreading and causing more significant harm. This rapid response is essential in controlling infections and ensuring they do not escalate into more severe conditions.
Repairing Damaged Tissues: Inflammation is equally important in the repair and regeneration of damaged tissues. When you sustain an injury, such as a cut or a sprain, the inflammatory response is activated. Blood flow to the injured area increases, delivering oxygen, nutrients, and essential cells that aid in tissue repair. Growth factors released during inflammation stimulate the production of new cells to replace those that were damaged. This process not only helps to heal the immediate injury but also strengthens the tissue to withstand future stress.
Examples of Beneficial Inflammation
Consider the common scenario of cutting your finger while preparing a meal. Almost immediately, the area around the cut becomes red, swollen, and warm. This acute inflammatory response is a sign that your body is working to protect and heal itself. The increased blood flow brings necessary nutrients and immune cells to the site, while the swelling helps to isolate the injury from further harm. Pain serves as a signal to protect the area, preventing further damage while it heals. Within a few days, you notice the cut starting to close and new skin forming, demonstrating the effectiveness of inflammation in the healing process.
Another example is the soreness and mild swelling you might experience after an intense workout. This type of inflammation is a natural response to microscopic muscle tears caused by physical exertion. The inflammatory process helps repair and strengthen the muscle fibers, leading to improved muscle function and growth over time.
Additionally, consider the redness and swelling that occur after an insect bite. The body’s immune system quickly responds to the foreign proteins injected by the insect, resulting in localized inflammation that helps neutralize the potential threat and start the healing process.
Finally, think about the temporary swelling and pain you might feel after a minor burn. This acute inflammation helps to prevent infection and promotes tissue repair, illustrating the body’s immediate and effective response to injury.
Table 2. Examples of Acute Inflammation
| Scenario | Symptoms | Purpose | Outcome |
|---|---|---|---|
| Cut Finger | Redness, swelling, warmth, pain | Brings nutrients and immune cells, isolates injury | Healing of the cut, formation of new skin |
| Intense Workout | Soreness, mild swelling | Repairs and strengthens muscle fibers | Improved muscle function and growth |
| Insect Bite | Redness, swelling | Neutralizes foreign proteins, starts healing | Neutralization of threat, start of healing |
| Minor Burn | Swelling, pain | Prevents infection, promotes tissue repair | Healing of burn, prevention of infection |
Inflammation is a fundamental aspect of the body’s natural defense mechanism. It acts quickly to eliminate threats and initiate healing, ensuring that we recover from injuries and infections. Without inflammation, our bodies would struggle to fight off infections, heal from injuries, or cope with the wear and tear of daily life.
In essence, inflammation is a protective response critical for maintaining health and resilience. By understanding the beneficial aspects of inflammation, we can appreciate its role in keeping us safe and facilitating recovery. Recognizing the difference between helpful and harmful inflammation is key to managing our health effectively and preventing chronic conditions.
While acute inflammation is a vital part of the body’s defense and healing processes, chronic inflammation tells a different story. When inflammation lingers for an extended period, it can lead to a host of health problems. Chronic inflammation occurs when the immune system continues to send out inflammatory responses even when there is no immediate threat. This persistent inflammation can damage healthy tissues and contribute to the development of various diseases.
Common Causes of Chronic Inflammation
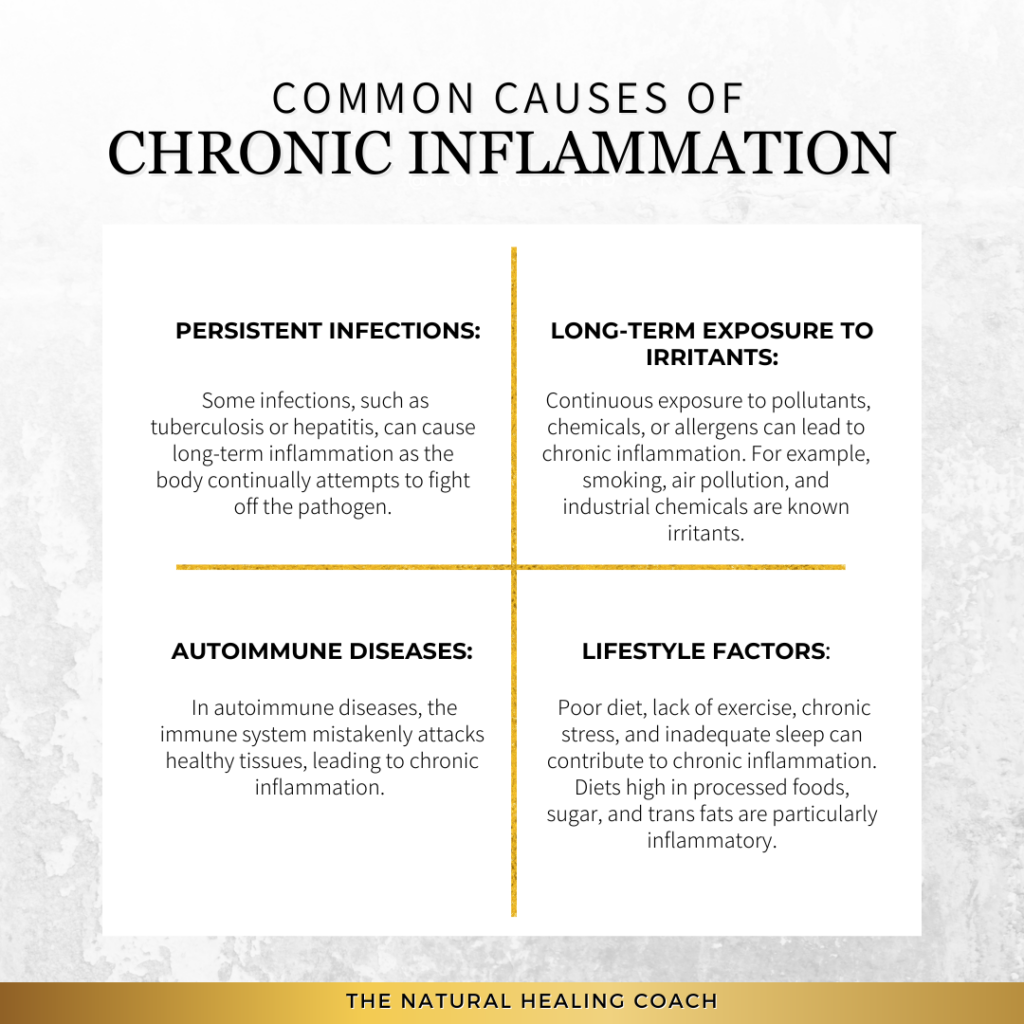
Persistent Infections: Some infections, such as tuberculosis or hepatitis, can cause long-term inflammation as the body continually attempts to fight off the pathogen.
Long-term Exposure to Irritants: Continuous exposure to pollutants, chemicals, or allergens can lead to chronic inflammation. For example, smoking, air pollution, and industrial chemicals are known irritants.
Autoimmune Diseases: In autoimmune diseases, the immune system mistakenly attacks healthy tissues, leading to chronic inflammation. Conditions such as rheumatoid arthritis, lupus, and multiple sclerosis are examples of autoimmune diseases characterized by chronic inflammation.
Lifestyle Factors: Poor diet, lack of exercise, chronic stress, and inadequate sleep can contribute to chronic inflammation. Diets high in processed foods, sugar, and trans fats are particularly inflammatory.
Health Conditions Associated with Chronic Inflammation
Cardiovascular Disease: Chronic inflammation plays a key role in the development of atherosclerosis, where inflamed blood vessels lead to plaque buildup, increasing the risk of heart attack and stroke.
Autoimmune Diseases: Conditions like rheumatoid arthritis, lupus, and inflammatory bowel disease are driven by chronic inflammation, leading to pain, tissue damage, and impaired function.
Diabetes: Chronic inflammation can contribute to insulin resistance, a precursor to type 2 diabetes. Inflammatory markers are often elevated in individuals with obesity, a major risk factor for diabetes.
Cancer: Persistent inflammation can damage DNA and lead to mutations, promoting the development and progression of certain cancers.
Neurodegenerative Diseases: Chronic inflammation in the brain is associated with neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease. Inflammation can exacerbate the damage to neurons and impair cognitive function.
Table 3. Inflammation Sites in Various Diseases
| Health Condition | Inflammation Site | Impact |
|---|---|---|
| Cardiovascular Disease | Blood Vessels | Plaque buildup, increased risk of heart attack and stroke |
| Autoimmune Diseases | Joints, Skin, Organs | Pain, tissue damage, impaired function |
| Diabetes | Pancreas, Blood Vessels | Insulin resistance, high blood sugar levels |
| Cancer | Various Tissues | DNA damage, tumor development and progression |
| Neurodegenerative Diseases | Brain | Neuron damage, cognitive impairment |
By understanding the causes and effects of chronic inflammation, we can better manage our health and take preventive measures to reduce its impact. Recognizing the difference between helpful and harmful inflammation is key to managing our health effectively and preventing chronic conditions.
The Impact of Chronic Inflammation on Overall Health
Chronic inflammation not only contributes to the development of serious diseases but also affects overall health and quality of life. Symptoms such as fatigue, pain, digestive issues, and mood disorders can all be linked to chronic inflammation. It creates a state of ongoing stress in the body, which can deplete energy, lower immunity, and impair the ability to recover from illnesses and injuries.
Understanding and addressing chronic inflammation is crucial for maintaining long-term health. This involves identifying and mitigating potential triggers, adopting a healthy lifestyle, and seeking appropriate medical care. By managing chronic inflammation, we can reduce the risk of associated diseases and improve overall well-being.
Inflammation is a complex biological process that is often misunderstood. Several myths and misconceptions about inflammation can lead to confusion about its role in health and disease. Let’s clarify these misunderstandings with evidence-based insights.
Myth 1: Inflammation is Always Harmful
Many people believe that all inflammation is harmful and should be suppressed at all costs. However, as we’ve discussed, acute inflammation is a crucial part of the body’s defense mechanism. It helps to isolate and eliminate harmful stimuli and initiate the healing process. Chronic inflammation, on the other hand, can be detrimental. Understanding the difference between beneficial acute inflammation and harmful chronic inflammation is essential for managing our health effectively
Myth 2: Anti-inflammatory Drugs Are Always the Best Solution
While anti-inflammatory drugs can be effective in reducing inflammation and relieving pain, they are not always the best solution. Overuse of these medications can lead to side effects such as gastrointestinal issues, increased risk of heart disease, and kidney damage. Additionally, they may not address the underlying cause of chronic inflammation. Lifestyle changes, such as improving diet, increasing physical activity, managing stress, and getting adequate sleep, can be more sustainable and holistic approaches to managing chronic inflammation.
Myth 3: Inflammation is the Same for Everyone
Inflammation can vary significantly from person to person based on genetics, lifestyle, environment, and overall health. For instance, some individuals may have a heightened inflammatory response due to genetic predispositions, while others may experience milder symptoms. It’s important to recognize that inflammation is a personalized experience, and what works for one person in managing it may not work for another
Myth 4: Diet Has No Significant Impact on Inflammation
Some people believe that diet has little to do with inflammation, but research shows that certain foods can significantly influence inflammatory processes in the body. Diets high in processed foods, sugar, and trans fats can promote inflammation, while diets rich in fruits, vegetables, whole grains, and omega-3 fatty acids can help reduce it. Understanding the impact of diet on inflammation can be a powerful tool in managing and preventing chronic inflammation.
Myth 5: Exercise Worsens Inflammation
While intense or excessive exercise can cause temporary inflammation, regular moderate exercise has been shown to reduce chronic inflammation. Physical activity helps to regulate immune function, reduce fat mass, and improve circulation, all of which can contribute to lowering chronic inflammation levels. It’s important to find a balance and engage in regular, moderate exercise to maintain overall health and manage inflammation.
Clarification of These Misconceptions
By debunking these myths, we can gain a clearer understanding of inflammation and its role in health. Acute inflammation is a protective response essential for healing, while chronic inflammation can lead to various health issues if left unchecked. Managing inflammation requires a holistic approach, including lifestyle changes and, when necessary, medical intervention. Recognizing that inflammation is a personalized experience helps tailor strategies to individual needs, ultimately leading to better health outcomes.
Managing Inflammation: Practical Tips and Strategies
Effectively managing inflammation involves a combination of dietary changes, lifestyle modifications, and natural remedies. By implementing these strategies, you can reduce chronic inflammation and improve your overall health.
Dietary Changes to Reduce Inflammation
Anti-inflammatory Foods Incorporating anti-inflammatory foods into your diet can help combat chronic inflammation. Some examples include:
- Fatty Fish: Rich in omega-3 fatty acids, which have been shown to reduce inflammation. Examples include salmon, mackerel, and sardines.
- Leafy Greens: Vegetables like spinach, kale, and collard greens are packed with antioxidants and vitamins that help fight inflammation.
- Nuts: Nuts such as almonds and walnuts contain healthy fats, fiber, and antioxidants that can reduce inflammation.
Foods to Avoid Certain foods can exacerbate inflammation and should be limited or avoided:
- Processed Foods: Foods high in trans fats, refined carbohydrates, and preservatives can trigger inflammation.
- Excessive Sugar: High sugar intake can increase inflammatory markers in the body.
- Refined Carbohydrates: White bread, pastries, and other refined carbs can contribute to inflammation.
Lifestyle Modifications
Stress Management Techniques Chronic stress can lead to increased inflammation. Managing stress is crucial for reducing inflammation. Techniques include:
- Mindfulness: Practicing mindfulness meditation can help reduce stress and lower inflammatory markers.
- Yoga: Yoga combines physical activity with mindfulness and deep breathing, which can reduce stress and inflammation.
Regular Physical Activity Engaging in regular exercise can help regulate immune function and reduce chronic inflammation. Types of exercise include:
- Moderate Exercise: Aim for at least 30 minutes of moderate exercise most days of the week. Activities like walking, swimming, and cycling are excellent choices.
Adequate Quality Sleep Getting enough sleep is essential for managing inflammation. Poor sleep can increase inflammatory markers in the body. Suggestions to improve sleep quality include:
- Aiming for 7-9 hours of quality sleep per night.
- Establishing a regular sleep routine and creating a restful sleep environment can help improve sleep quality.
Natural Remedies and Supplements for Inflammation
Turmeric Turmeric contains curcumin, a compound with potent anti-inflammatory properties. Adding turmeric to your diet or taking a curcumin supplement can help reduce inflammation.
Omega-3 Fatty Acids Omega-3 fatty acids, found in fish oil supplements and fatty fish, are known for their anti-inflammatory effects. They can help lower inflammation and improve overall health.
Other Supplements
- Ginger: Known for its anti-inflammatory and antioxidant properties.
- Green Tea: Contains anti-inflammatory compounds that can help reduce inflammation.
- Probiotics: Beneficial for gut health, which is closely linked to inflammation.
Importance of Consulting Healthcare Professionals
While dietary changes, lifestyle modifications, and natural remedies can significantly reduce inflammation, it’s essential to consult with healthcare professionals for personalized advice. They can help identify the underlying causes of inflammation and recommend appropriate treatments. If you’re considering supplements, it’s particularly important to discuss them with your healthcare provider to ensure they are safe and suitable for your individual needs.
By integrating these practical tips and strategies into your daily routine, you can effectively manage inflammation and enhance your overall well-being.
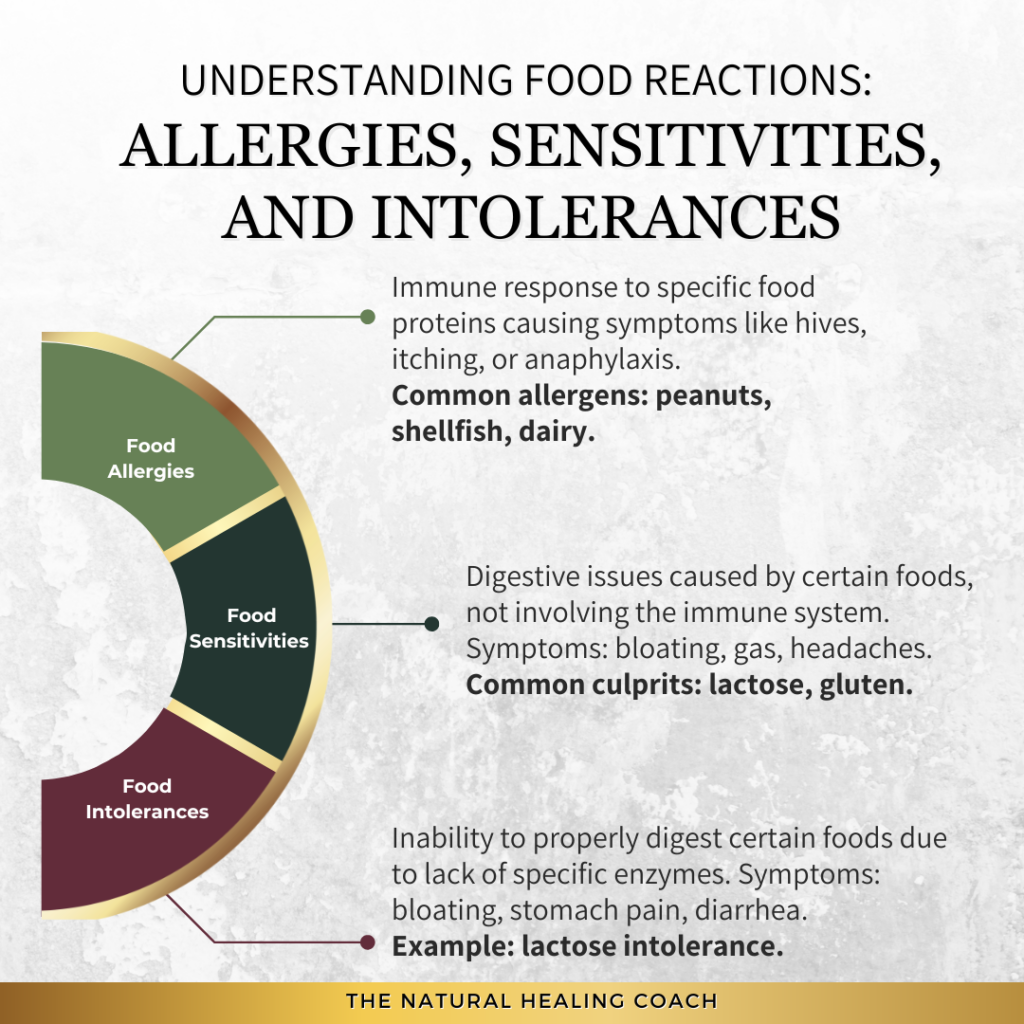
A Deeper Dive Into Autoimmune Disease in Inflammatory Responses
Autoimmune diseases play a significant role in chronic inflammation. In these conditions, the body’s immune system mistakenly attacks its own tissues, leading to persistent and often debilitating inflammation. This chronic inflammatory response, intended to protect the body, causes more harm than good in autoimmune diseases.
Autoimmune diseases occur when the immune system fails to differentiate between healthy cells and harmful invaders, such as bacteria and viruses. This misidentification triggers an immune response against the body’s own tissues, resulting in chronic inflammation. Understanding how autoimmune diseases trigger this harmful inflammation and how to manage it is crucial for those affected.
Table 4. Specific Examples of Autoimmune Diseases
| Disease | Description | Impact |
|---|---|---|
| Rheumatoid Arthritis (RA) | A chronic inflammatory disorder affecting the joints. | Causes painful swelling, bone erosion, and joint deformity. |
| Systemic Lupus Erythematosus (SLE) | An autoimmune disease where the immune system attacks its own tissues. | Affects skin, joints, kidneys, brain, and other organs. |
| Psoriasis | A chronic skin condition characterized by red, scaly patches. | Can cause significant discomfort and psychological stress. |
| Multiple Sclerosis (MS) | A disease where the immune system attacks the protective sheath (myelin). | Can cause permanent nerve damage and disability. |
| Inflammatory Bowel Disease (IBD) | Includes Crohn’s disease and ulcerative colitis. | Leads to severe diarrhea, pain, fatigue, and weight loss. |
| Ankylosing Spondylitis (AS) | A form of arthritis that primarily affects the spine. | Causes inflammation of the spinal joints, leading to severe pain. |
| Type 1 Diabetes | An autoimmune condition where the immune system attacks insulin-producing cells. | Requires lifelong insulin therapy, can lead to serious complications. |
| Hashimoto’s Thyroiditis | An autoimmune disorder where the immune system attacks the thyroid gland. | Leads to hypothyroidism, affecting metabolism and energy levels. |
| Celiac Disease | An autoimmune disorder where the ingestion of gluten leads to small intestine damage. | Causes digestive issues and malabsorption of nutrients. |
| Sjogren’s Syndrome | An autoimmune disease that attacks the glands producing tears and saliva. | Causes dry eyes, dry mouth, and can affect other organs. |
Disease-Specific Strategies for Managing Autoimmune Disease
When dealing with autoimmune diseases, it might seem practical to offer universal tips for managing inflammation. However, each autoimmune condition has unique characteristics, affected organs, and symptom patterns that require specific approaches for effective management. Here’s a closer look at why disease-specific strategies are crucial.
Disease-Specific Factors
1. Target Organs and Systems
Autoimmune diseases impact different organs and systems. For instance:
- Rheumatoid Arthritis: Primarily affects the joints, causing pain and swelling.
- Multiple Sclerosis: Targets the central nervous system, leading to neurological symptoms.
- Hashimoto’s Thyroiditis: Impacts the thyroid, leading to hormonal imbalances.
Each of these conditions requires targeted inflammation management strategies to address the specific areas affected.
2. Symptoms
The symptoms of autoimmune diseases can vary widely:
- Sjögren’s Syndrome: Characterized by dry eyes and mouth.
- Celiac Disease: Involves gastrointestinal issues such as bloating and diarrhea.
Inflammation reduction strategies should be tailored to alleviate the distinct symptoms for each of these conditions, as a one-size-fits-all approach might not address the unique challenges of each condition.
3. Triggers and Aggravators
Different autoimmune diseases have varying triggers:
- Celiac Disease: Gluten triggers severe symptoms.
- Lupus: Sun exposure can exacerbate the condition.
Inflammation mitigation strategies must include avoiding or mitigate these specific triggers to prevent flare-ups.
Individualized Management
- Diet
While anti-inflammatory diets can benefit many autoimmune conditions, specific dietary needs differ:
- Celiac Disease: Requires a strict gluten-free diet.
- Rheumatoid Arthritis: Might benefit from an anti-inflammatory diet rich in omega-3 fatty acids.
It’s essential to tailor dietary recommendations to the specific needs of each disease for effective management.
2. Exercise
Exercise recommendations also vary:
- Rheumatoid Arthritis: Low-impact exercises like swimming or yoga are often advised to reduce joint stress.
- Ankylosing Spondylitis (AS): Regular physical activity is crucial to prevent spinal fusion.
These differences underscore the importance of personalized exercise plans based on the disease’s impact on the body.
3. Medications
Medication regimens for autoimmune diseases can differ significantly:
- RA: Often requires immunosuppressants or biologics.
- Hashimoto’s Thyroiditis: May need hormone replacement therapy.
- Type 1 Diabetes: Requires insulin management.
Understanding these differences is crucial for effective medication management and overall disease control.
Other Influencing Factors
Managing inflammation in autoimmune conditions requires a multifaceted approach. Here are some general tips:
By understanding the role of autoimmune diseases in chronic inflammation and implementing these management strategies, individuals can better control their symptoms, reduce inflammation, and improve their quality of life.
Final Thoughts
Inflammation is a complex process with both beneficial and harmful effects. While acute inflammation is essential for healing and defense, chronic inflammation can lead to a host of health problems, particularly in the context of autoimmune diseases. Understanding the nuances of inflammation helps us recognize its vital role in our bodies and the importance of managing it effectively.
By making informed dietary choices, adopting a healthy lifestyle, and utilizing natural remedies, we can significantly reduce chronic inflammation and improve our overall well-being. Additionally, it’s crucial for individuals with autoimmune conditions to work closely with healthcare professionals to tailor their treatment plans and manage inflammation effectively.
Recognizing the difference between helpful and harmful inflammation empowers us to take proactive steps toward better health. Embracing these strategies not only helps in managing chronic inflammation but also enhances our quality of life.
Call to Action
If you found this information helpful and want to learn more about managing autoimmune conditions and staying active, we invite you to engage with our community. Join the conversation, share your experiences, and connect with others who are on the same journey towards better health.
Stay Informed and Connected
- Engage on Social Media: Follow us on your favorite social media platforms for daily tips, inspiration, and community support. We regularly share practical advice, uplifting stories, and the latest research on exercising with autoimmune conditions. Join the conversation and be part of a supportive community.
Subscribe to Our Newsletter
- Exclusive Insights: Get in-depth articles and updates on the latest research in autoimmune health directly to your inbox.
- Health Tips: Receive practical tips and strategies for managing your condition and improving your overall well-being.
- Stay Updated: Be the first to know about new blog posts, upcoming events, and other valuable resources.
Join the Discussion
- Leave a Comment: We’d love to hear your thoughts and experiences. Share your insights in the comments below and connect with others who are on the same journey. Your comments help build a supportive community where everyone can learn and grow together.
Together, we can take proactive steps towards better health and well-being, even with autoimmune disease.
If you are looking for more tips and support, join me over on my group page, The Village – A Natural HEALing Community, to get tons of information and tips to help you take your HEALTHY EATING and ACTIVE LIVING to the next level.
REFERENCES:
- Elimination Diets: A Comprehensive Overview – Healthline
- Nutrition and Immunology: The Impact of Diet on Immune Function – Harvard T.H. Chan School of Public Health
- Why and How To Start an Elimination Diet – Cleveland Clinic
- Autoimmune Diseases and the Benefits of Elimination Diets – National Institute of Allergy and Infectious Diseases (NIAID)
- Efficacy of Elimination Diets in Eosinophilic Esophagitis – Journal of Clinical Gastroenterology
- Mayo Clinic. (2021). Food Allergy.
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Lactose Intolerance.
- National Center for Biotechnology Information. (2014). The Autoimmune Protocol Diet Modifies Intestinal Microbiota.
MORE RELATED POSTS:








+leave a comment . . .