Introduction
Imagine waking up every morning with itchy, red patches on your skin, feeling self-conscious and in constant discomfort. This is the daily reality for many individuals living with psoriasis. The persistent itching and visible patches can significantly impact one’s quality of life, leading to emotional distress and social isolation. Understanding psoriasis, its symptoms, causes, and management strategies is crucial for those affected and their support systems.
Psoriasis affects millions of people worldwide. In the United States, around 7.5 million people are affected by psoriasis. Share on XGlobally, approximately 2-3% of the population suffers from this condition, with varying prevalence in different regions. The distribution of psoriasis can differ by age, gender, and ethnicity, with higher prevalence observed in adults compared to children. It is equally common in men and women; however, certain ethnic groups, such as Caucasians, are more frequently affected than others.
Understanding Psoriasis and Its Symptoms
Psoriasis Symptoms
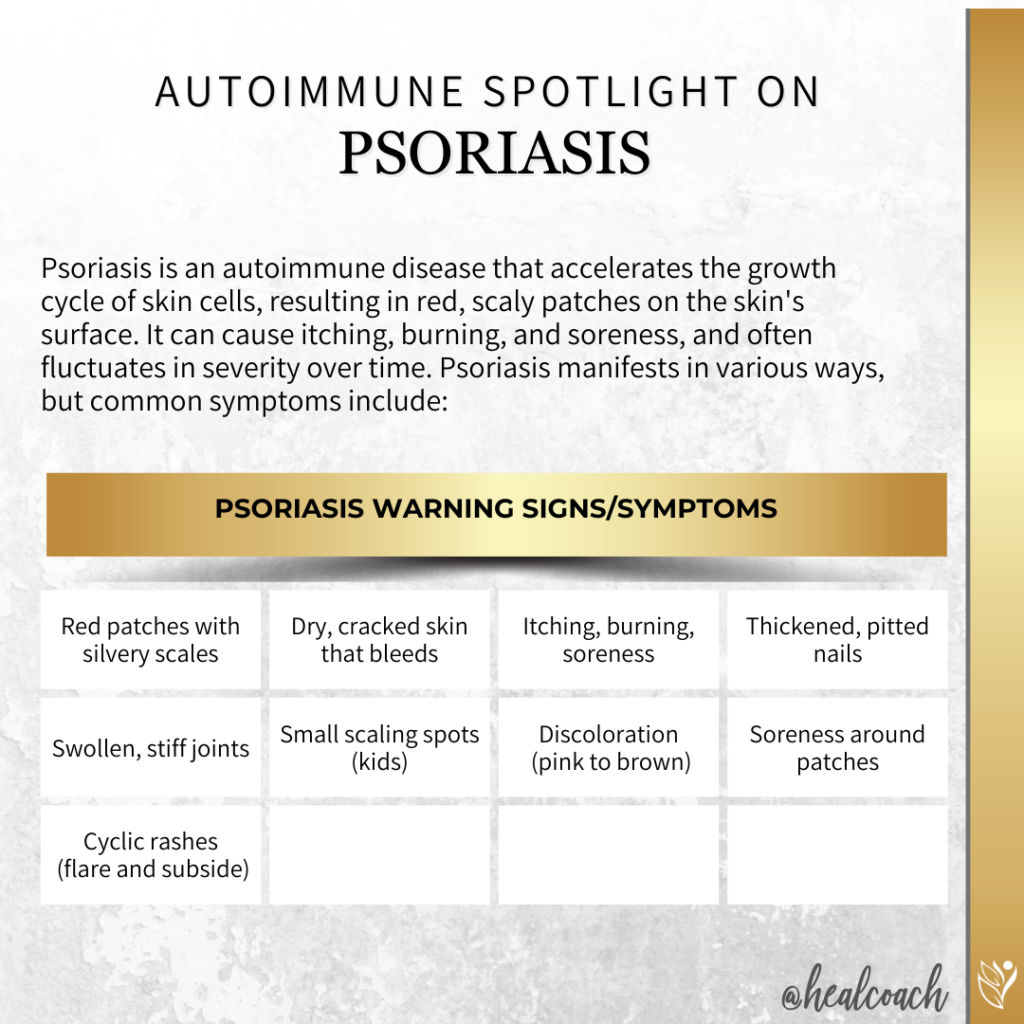
Psoriasis is an autoimmune disease that accelerates the production of skin cells, leading to a rapid buildup on the skin’s surface. This results in red patches covered with thick, silvery scales that can be itchy and sometimes painful. Far from being merely a cosmetic issue, psoriasis is a persistent, long-lasting condition that can fluctuate in severity over time.
Psoriasis manifests in various ways, but common symptoms include red patches of skin covered with thick, silvery scales, dry and cracked skin that may bleed, and intense itching, burning, or soreness.
Types of Psoriasis
There are several types of psoriasis, each with its unique characteristics:
| Type | Characteristics |
|---|---|
| Plaque Psoriasis | The most common form, accounting for about 80-90% of cases. It is characterized by raised, red patches with a silvery white buildup of dead skin cells, often appearing on the elbows, knees, scalp, and lower back. |
| Guttate Psoriasis | Often starting in childhood or young adulthood, this type presents as small, dot-like lesions. Guttate psoriasis can be triggered by infections, such as strep throat. |
| Inverse Psoriasis | Appearing as bright red, shiny lesions, this type typically affects skin folds such as under the breasts, in the groin, or around the buttocks. It is more common in overweight individuals and can be exacerbated by friction and sweating. |
| Pustular Psoriasis | Characterized by white pustules (blisters of non-infectious pus) surrounded by red skin. It can occur on any part of the body but is most common on the hands or feet. |
| Erythrodermic Psoriasis | A particularly severe form that can cover large portions of the body with a red, peeling rash that can itch or burn intensely. This type can be life-threatening and often requires immediate medical attention. |
Understanding these types of psoriasis and their symptoms is crucial for managing the condition and seeking appropriate treatment.
Causes of Psoriasis
Because psoriasis is an autoimmune condition, it arises from an abnormal response of the body’s immune system. In psoriasis, the immune system mistakenly attacks healthy skin cells, accelerating their production and causing a rapid buildup on the skin’s surface.
Genetic Predisposition and Environmental Triggers
Genetics play a significant role in the development of psoriasis. If a parent has psoriasis, their child has a higher likelihood of developing the condition. However, having a genetic predisposition alone is not enough; environmental triggers often play a crucial role in the onset of psoriasis symptoms.
Common environmental triggers include:
- Infections: Streptococcal infections, particularly strep throat, are known to trigger guttate psoriasis.
- Injury to the Skin: Cuts, scrapes, sunburns, or even vaccinations can provoke a psoriasis outbreak, a phenomenon known as the Koebner response.
- Stress: High levels of stress can weaken the immune system, potentially triggering or worsening psoriasis.
- Weather: Cold, dry weather can exacerbate symptoms, while warm, sunny climates can sometimes improve them.
- Lifestyle Factors: Smoking and heavy alcohol consumption can increase the risk of developing psoriasis or trigger flare-ups.
Immune System Attack on Healthy Skin Cells
In individuals with psoriasis, the immune system’s T cells, which typically defend the body against infections, mistakenly attack healthy skin cells. This attack triggers a cascade of immune responses, leading to inflammation and the rapid turnover of skin cells. Normally, skin cells renew every 28-30 days, but in psoriasis, this process accelerates to every 3-4 days. The result is a buildup of dead skin cells on the surface, forming the characteristic scales and red patches.
Understanding these causes and triggers is essential for managing psoriasis effectively. Identifying and avoiding personal triggers, along with medical treatment, can help control the condition and improve the quality of life for those affected.
Risk Factors for Psoriasis
Several factors can increase the risk of developing psoriasis or trigger flare-ups in those who already have the condition. These risk factors include:
Genetic Factors and Family History
A strong genetic component is associated with psoriasis. If one or both parents have psoriasis, their children are at a higher risk of developing the condition. Studies have shown that certain genes are linked to psoriasis, although the exact genetic pathways are still being researched.
Lifestyle Factors
Certain lifestyle choices can contribute to the development or exacerbation of psoriasis:
- Stress: High levels of stress can weaken the immune system and trigger or worsen psoriasis symptoms.
- Smoking: Tobacco use is a known risk factor for the onset and severity of psoriasis. Smokers are more likely to develop psoriasis, and the condition tends to be more severe in those who smoke.
- Alcohol Consumption: Heavy alcohol use can increase the risk of psoriasis and can make treatment less effective.
Other Medical Conditions
Several medical conditions and external factors can increase the risk of psoriasis:
- Infections: Bacterial and viral infections, particularly streptococcal throat infections, can trigger psoriasis in some individuals.
- Skin Injuries: Cuts, scrapes, sunburns, or other injuries to the skin can provoke a psoriasis outbreak. This response is known as the Koebner phenomenon.
- Certain Medications: Some drugs, including lithium, beta-blockers, and antimalarials, can trigger or exacerbate psoriasis.
- Obesity: Excess weight increases the risk of psoriasis and can make the condition more severe. Plaques associated with all types of psoriasis often develop in skin creases and folds.
Understanding and managing these risk factors can help reduce the likelihood of developing psoriasis or experiencing severe flare-ups. This awareness is crucial for individuals with a family history of psoriasis or those who exhibit other risk factors.
Diagnosis of Psoriasis
Diagnosing psoriasis involves several key steps to ensure an accurate identification of the condition and to differentiate it from other skin disorders.
Steps Involved in Diagnosing Psoriasis
Importance of Differentiating Psoriasis from Other Skin Conditions
Accurately diagnosing psoriasis is crucial because its symptoms can resemble those of other skin conditions, such as eczema, fungal infections, or seborrheic dermatitis. Differentiating psoriasis from these conditions is essential for several reasons:
- Appropriate Treatment: Different skin conditions require different treatment approaches. Accurate diagnosis ensures that the patient receives the most effective therapy for their specific condition.
- Avoiding Complications: Misdiagnosis can lead to inappropriate treatments that might not only be ineffective but could also exacerbate the condition or cause additional health issues.
- Managing Expectations: Understanding that psoriasis is a chronic, autoimmune condition helps patients set realistic expectations about managing the disease and its symptoms over the long term.
Through a combination of physical examination, medical history, and diagnostic tests like skin biopsies, healthcare providers can accurately diagnose psoriasis and develop a tailored treatment plan to manage the condition effectively.
Treatment Options for Psoriasis
Managing psoriasis effectively involves a range of treatment strategies, tailored to the severity of the condition and the patient’s specific needs. Here is an overview of the primary treatment options:
Topical Treatments
Topical treatments are often the first line of defense for mild to moderate psoriasis. These include creams and ointments applied directly to the skin to reduce inflammation, remove scales, and slow the rapid turnover of skin cells.
- Corticosteroids: These are anti-inflammatory drugs that can reduce swelling and redness. They are commonly prescribed for mild to moderate psoriasis.
- Vitamin D Analogues: These synthetic forms of vitamin D can slow the growth of skin cells.
- Retinoids: Derived from vitamin A, these compounds help reduce inflammation and slow skin cell growth.
- Salicylic Acid: This helps remove scales and smooth the skin.
- Coal Tar: This traditional treatment can reduce scaling, itching, and inflammation.
Systemic Medications
For moderate to severe psoriasis or when topical treatments are not effective, systemic medications may be prescribed. These drugs work throughout the body and can be administered orally or by injection.
- Oral Medications:
- Methotrexate: Reduces inflammation and slows skin cell production.
- Cyclosporine: Suppresses the immune system to slow skin cell turnover.
- Acitretin: A retinoid that helps control skin cell growth.
- Biologics: These are newer medications made from living organisms. They target specific parts of the immune system.
- Examples include adalimumab (Humira), etanercept (Enbrel), and ustekinumab (Stelara).
Phototherapy (Light Therapy)
Phototherapy involves exposing the skin to controlled amounts of natural or artificial ultraviolet (UV) light. This treatment can reduce symptoms by slowing skin cell turnover and reducing inflammation.
- UVB Phototherapy: Uses UVB light, which penetrates the outer layer of skin.
- PUVA: Combines UVA light with a drug called psoralen to make the skin more sensitive to light.
- Excimer Laser: Targets specific areas of skin with high-intensity UVB light.
Complementary and Alternative Therapies
In addition to conventional treatments, some patients find relief through complementary and alternative therapies. These can be used in conjunction with traditional treatments but should always be discussed with a healthcare provider.
- Dietary Supplements: Omega-3 fatty acids, vitamin D, and other supplements may help reduce inflammation.
- Herbal Remedies: Aloe vera, tea tree oil, and other herbal treatments can soothe the skin.
- Mind-Body Techniques: Stress reduction techniques such as yoga, meditation, and acupuncture can help manage psoriasis symptoms by reducing stress.
- Diet and Lifestyle Changes: Maintaining a healthy diet, avoiding triggers like smoking and alcohol, and staying active can help manage symptoms.
A comprehensive treatment plan for psoriasis may involve a combination of these strategies, tailored to the individual’s needs and the severity of their condition. It’s important for patients to work closely with their healthcare provider to find the most effective and appropriate treatment regimen.
Living with and Flare Management for Psoriasis
Living with psoriasis requires ongoing attention to daily routines and proactive strategies to manage and prevent flare-ups. Here are some essential tips for managing psoriasis effectively:
Daily Management Tips
Skincare Routines
- Moisturizing: Keeping the skin well-hydrated is crucial. Use thick, fragrance-free moisturizers to prevent dryness and cracking.
- Gentle Cleansing: Use mild soaps and avoid hot water, which can dry out the skin. Pat your skin dry with a soft towel instead of rubbing it.
Avoiding Triggers
- Identify and Avoid Triggers: Keep a diary to track and identify what might trigger your psoriasis, such as certain foods, stress, or weather changes.
- Sun Protection: While moderate sun exposure can help some people, it’s important to protect your skin from sunburn, which can trigger flare-ups. Use sunscreen with at least SPF 30.
Strategies for Managing Flares
Stress Reduction
- Mindfulness and Relaxation Techniques: Practices like yoga, meditation, and deep-breathing exercises can help reduce stress levels.
- Regular Exercise: Physical activity can improve overall health and reduce stress, but be sure to choose low-impact exercises that do not irritate the skin.
Diet and Lifestyle Changes
- Healthy Diet: A balanced diet rich in fruits, vegetables, lean proteins, and healthy fats can support overall health and potentially reduce inflammation. Some people find that specific diets, such as Autoimmune Protocol Diet (AIP), help manage their symptoms.
- Avoiding Alcohol and Smoking: Both alcohol and smoking can worsen psoriasis symptoms. Reducing or eliminating these can help manage the condition.
Importance of Support Systems and Mental Health Management
Living with psoriasis can be challenging, both physically and emotionally. Support systems and mental health management are crucial components of comprehensive care.
Support Systems
- Join Support Groups: Connecting with others who have psoriasis can provide emotional support and practical advice. Consider joining a local or online support group.
- Communicate with Loved Ones: Educate your family and friends about psoriasis to help them understand your condition and provide better support.
Mental Health Management
- Professional Help: If psoriasis impacts your mental health, consider talking to a mental health professional. Therapy can provide strategies for coping with the emotional aspects of living with a chronic condition.
- Stress Management: Incorporate stress-reducing activities into your daily routine, such as hobbies, reading, or spending time in nature.
By integrating these daily management tips, flare management strategies, and emphasizing support systems and mental health, individuals with psoriasis can improve their quality of life and better control their condition. Working closely with healthcare providers to tailor these approaches to personal needs is essential for effective management.
Emerging Research in Psoriasis
The field of psoriasis research is continuously evolving, with new studies and advancements enhancing our understanding of the condition and improving treatment options. Here are some of the latest developments:
Current Studies and Advancements in Understanding Psoriasis
Researchers are making significant strides in understanding the underlying mechanisms of psoriasis. Recent studies have identified specific genetic markers and immune system pathways involved in the development and progression of the disease. Key areas of focus include:
- Genetic Research: Identifying genes associated with psoriasis to better understand hereditary factors and potential genetic targets for treatment.
- Immune System Pathways: Exploring how the immune system’s T cells and cytokines contribute to the rapid turnover of skin cells. This research is crucial for developing targeted therapies.
- Microbiome Studies: Investigating the role of the skin and gut microbiome in psoriasis. Understanding the interaction between microbes and the immune system may lead to new treatment approaches.
New Treatment Options and Therapies Being Developed
Innovative treatment options are continually being developed, offering hope for more effective management of psoriasis. Some of the promising new therapies include:
- Biologics: Newer biologic drugs target specific components of the immune system, such as interleukins and TNF-alpha, with fewer side effects than traditional systemic treatments. Examples include guselkumab (Tremfya) and risankizumab (Skyrizi).
- Small Molecule Inhibitors: Oral medications like apremilast (Otezla) inhibit specific molecules involved in the inflammatory process, providing an alternative to biologics and traditional systemic treatments.
- Topical Treatments: Advances in topical treatments include the development of new formulations that enhance the penetration and efficacy of active ingredients while minimizing side effects. For instance, non-steroidal creams like tapinarof and roflumilast are showing promise in clinical trials.
- Phototherapy Innovations: Improvements in phototherapy techniques, such as targeted UVB devices and combination therapies with topical agents, are enhancing the effectiveness and convenience of light therapy.
The Role of Personalized Medicine in Treating Psoriasis
Personalized medicine is becoming increasingly important in the treatment of psoriasis. By tailoring treatments to an individual’s genetic makeup, lifestyle, and specific disease characteristics, personalized medicine aims to improve outcomes and reduce side effects. Key aspects include:
- Genetic Profiling: Using genetic tests to identify the most effective treatments based on a patient’s genetic predisposition and specific immune system responses.
- Biomarker Research: Identifying biomarkers that predict treatment response and disease progression, allowing for more precise and effective therapy adjustments.
- Customized Treatment Plans: Developing individualized treatment plans that consider a patient’s overall health, lifestyle, and preferences, ensuring a holistic approach to managing psoriasis.
As research continues to advance, the future of psoriasis treatment looks promising, with the potential for more effective, targeted, and personalized therapies. Staying informed about these developments can help patients and healthcare providers make the best decisions for managing the condition.
Myths and Facts About Psoriasis
There are many misconceptions about psoriasis that can lead to misunderstanding and stigma. Here are some common myths and the facts that dispel them:
Common Misconceptions About Psoriasis
- Myth: Psoriasis is just a skin condition.
- Fact: Psoriasis is an autoimmune disease that affects the entire body. While it manifests on the skin, it is a systemic condition that can also impact joints and other organs.
- Myth: Psoriasis is contagious.
- Fact: Psoriasis is not contagious. You cannot catch psoriasis from someone else through physical contact, sharing items, or being close to them.
- Myth: Psoriasis only affects adults.
- Fact: Psoriasis can affect individuals of all ages, including children. Although it is more commonly diagnosed in adults, it can develop at any stage of life.
- Myth: Poor hygiene causes psoriasis.
- Fact: Psoriasis is not caused by poor hygiene. It is an autoimmune condition with genetic and environmental triggers, unrelated to cleanliness or personal hygiene.
- Myth: Psoriasis is a minor, cosmetic problem.
- Fact: Psoriasis can significantly impact a person’s quality of life, causing physical discomfort, emotional distress, and social isolation. Severe cases can lead to serious complications, such as psoriatic arthritis.
- Myth: There is a cure for psoriasis.
- Fact: Currently, there is no cure for psoriasis. However, there are many effective treatments available that can help manage the symptoms and improve quality of life.
By dispelling these myths and providing accurate information, we can foster a more informed and empathetic understanding of psoriasis, leading to better support and treatment for those living with this challenging condition.
Support and Resources for Psoriasis
Finding support and accessing reliable resources can make a significant difference in managing psoriasis. Here are some organizations, support groups, online communities, and educational resources for individuals with psoriasis:
Organizations
- National Psoriasis Foundation (NPF):
- Provides comprehensive support, patient education, advocacy, and research funding for psoriasis.
- www.psoriasis.org
- American Academy of Dermatology (AAD):
- Offers information on psoriasis treatment options, research updates, and connects patients with dermatologists.
- www.aad.org
- International Federation of Psoriasis Associations (IFPA):
- Works globally to improve the quality of life for people with psoriasis through advocacy, awareness, and research initiatives.
- www.ifpa-pso.com
Online Communities and Forums
- Psoriasis Support Community (Inspire):
- An online platform for sharing experiences, asking questions, and offering support.
- www.inspire.com/groups/psoriasis-support-community
- Reddit Psoriasis Community:
- A subreddit where individuals with psoriasis share advice, personal stories, and support.
- www.reddit.com/r/Psoriasis
- MyPsoriasisTeam:
- A social network for people with psoriasis to connect, share tips, and find support.
- www.mypsoriasisteam.com
Educational Resources
- Mayo Clinic Psoriasis Guide:
- Offers a comprehensive guide on psoriasis, including symptoms, causes, diagnosis, and treatment options.
- www.mayoclinic.org/diseases-conditions/psoriasis
- American Academy of Dermatology Psoriasis Resource Center:
- Provides detailed information on psoriasis management, treatment, and research updates.
- www.aad.org/public/diseases/psoriasis
Podcasts
- “Psound Bytes” by the National Psoriasis Foundation:
- A podcast that covers a range of topics related to psoriasis and psoriatic arthritis, including treatment options, research updates, and personal stories.
- Listen on: Podcast Site
- “The Psoriasis Geek Podcast”:
- Focuses on living with psoriasis, featuring interviews with experts, patient stories, and practical tips for managing the condition.
- Listen on: Podbean
- “The Autoimmune Wellness Podcast”:
- While not solely focused on psoriasis, this podcast covers a broad range of autoimmune conditions and offers valuable insights into holistic health and wellness strategies.
- Listen on: Autoimmune Wellness
Final Thoughts
Living with psoriasis can be challenging, but it is important to remember that you are not alone. Advances in research, new treatment options, and a growing community of support provide hope and encouragement for those managing this condition. By understanding psoriasis and taking proactive steps to manage your health, you can improve your quality of life.
Reach out to support groups and online communities, stay informed about the latest research and treatment options, and work closely with your healthcare providers to develop a personalized management plan. With the right resources and support, you can navigate the challenges of psoriasis and live a fulfilling life.
Call to Action
If you found this information helpful and want to learn more about managing autoimmune conditions and staying active, we invite you to engage with our community. Join the conversation, share your experiences, and connect with others who are on the same journey towards better health.
Stay Informed and Connected
- Engage on Social Media: Follow us on your favorite social media platforms for daily tips, inspiration, and community support. We regularly share practical advice, uplifting stories, and the latest research on exercising with autoimmune conditions. Join the conversation and be part of a supportive community.
Subscribe to Our Newsletter
- Exclusive Insights: Get in-depth articles and updates on the latest research in autoimmune health directly to your inbox.
- Health Tips: Receive practical tips and strategies for managing your condition and improving your overall well-being.
- Stay Updated: Be the first to know about new blog posts, upcoming events, and other valuable resources.
Join the Discussion
- Leave a Comment: We’d love to hear your thoughts and experiences. Share your insights in the comments below and connect with others who are on the same journey. Your comments help build a supportive community where everyone can learn and grow together.
Together, we can take proactive steps towards better health and well-being, even with autoimmune disease.
If you are looking for more tips and support, join me over on my group page, The Village – A Natural HEALing Community, to get tons of information and tips to help you take your HEALTHY EATING and ACTIVE LIVING to the next level.
REFERENCES:
- Mayo Clinic. Psoriasis.
- National Psoriasis Foundation. About Psoriasis.
- American Academy of Dermatology. Psoriasis Resource Center.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. Psoriasis.
- Healthline. Psoriasis: Symptoms, Causes, and Treatments.
MORE RELATED POSTS:







+leave a comment . . .