Introduction
Hashimoto’s disease, a leading cause of hypothyroidism, affects approximately 5 in 100 people in the United States alone, making it one of the most common autoimmune disorders. Despite its prevalence, Hashimoto’s often goes undiagnosed for years, leaving many individuals struggling with symptoms they don’t immediately connect to a thyroid condition.
Imagine waking up every morning feeling utterly drained, even after what should have been a restful night of sleep. Your energy levels are so low that simple daily tasks feel overwhelming. Despite no significant changes in your diet or exercise routine, the number on the scale keeps creeping up, and you can’t seem to shed the extra weight no matter what you try.
On top of that, you’re always cold, reaching for a sweater even on warm days, and your hair seems to be thinning at an alarming rate. These symptoms—persistent fatigue, unexplained weight gain, cold intolerance, and hair loss—are common experiences for those living with Hashimoto’s disease. Yet, they are often mistaken for signs of aging, stress, or other health issues, delaying proper diagnosis and treatment.
Hashimoto’s was the first autoimmune disease I was diagnosed with in 2015, a turning point in my health journey. Understanding this condition not only helped me manage my symptoms more effectively but also guided me to a path of advocacy and education for others experiencing similar struggles.
The purpose of this blog post is to provide an understanding of Hashimoto’s disease, its symptoms, causes, and effective management strategies. By shedding light on this often misunderstood condition, I aim to empower you with the knowledge needed to recognize the signs, seek appropriate medical care, and take proactive steps toward managing your health.
Understanding Hashimoto's isn't just about recognizing the symptoms—it's about learning how to live well with the disease and reducing its impact on your daily life. #healcoach #hashimotos #autoimmune Share on XThis blog post will explore the intricacies of Hashimoto’s, from diagnosis to treatment options, and offer practical advice on managing flare-ups and improving your overall well-being.
Understanding Hashimoto’s and Its Symptoms
To effectively manage Hashimoto’s disease, it’s crucial first to understand what it is and how it manifests in the body. By recognizing the symptoms early on, you can seek timely intervention and minimize the impact on your health.
What is Hashimoto’s Disease?
Hashimoto’s disease, also known as Hashimoto’s thyroiditis, is an autoimmune disorder in which the body’s immune system mistakenly attacks the thyroid gland. The thyroid, a small butterfly-shaped gland located at the base of your neck, plays a vital role in regulating metabolism, energy levels, and overall hormonal balance. In Hashimoto’s, the immune attack leads to inflammation and gradual destruction of the thyroid tissue, resulting in reduced thyroid hormone production, known as hypothyroidism.
Common Symptoms of Hashimoto’s
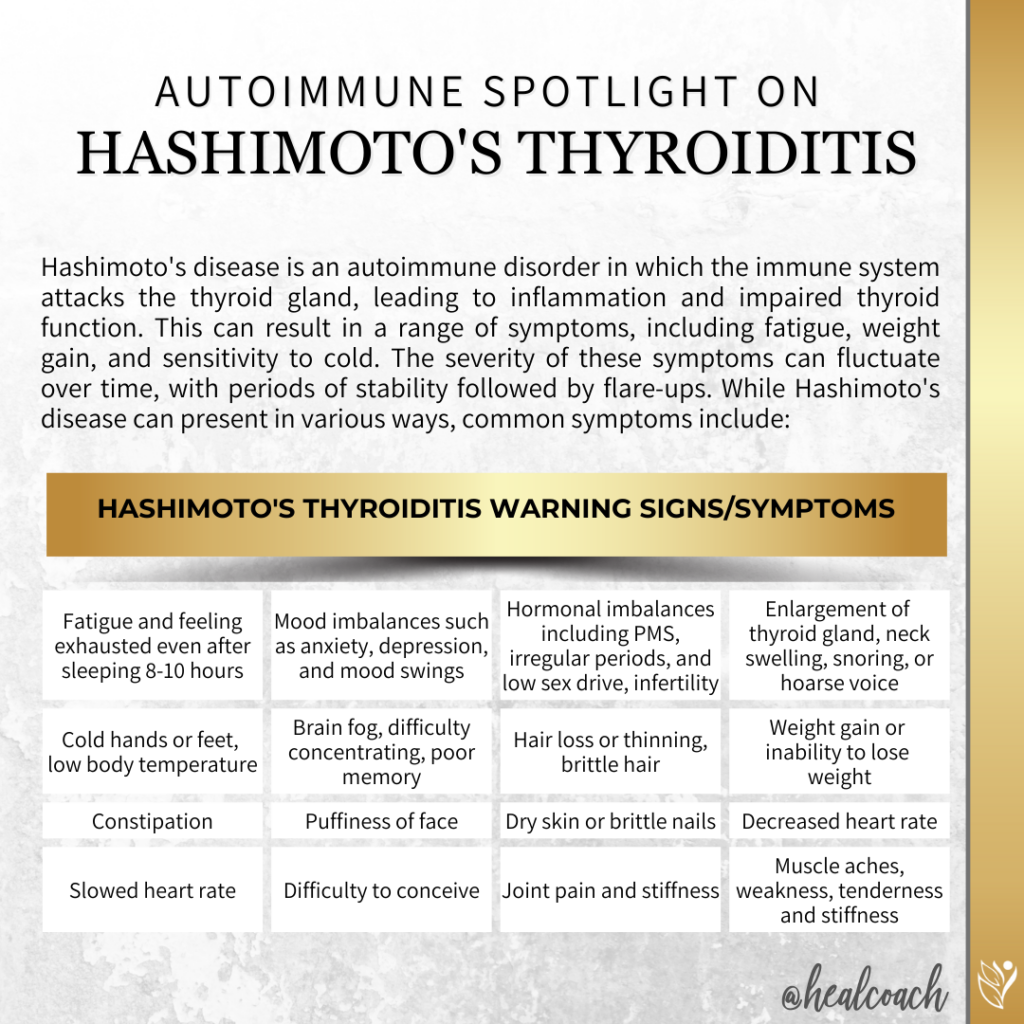
The symptoms of Hashimoto’s disease can be varied and often develop slowly over time. Some of the most common symptoms include persistent fatigue and exhaustion, even after a full night’s sleep. Many individuals experience mood imbalances such as anxiety, depression, and mood swings, along with hormonal issues like PMS, irregular periods, low sex drive, infertility, and difficulty conceiving. The thyroid gland may become enlarged, causing neck swelling, snoring, or a hoarse voice. Cold sensitivity is another frequent symptom, manifesting as cold hands or feet and a generally low body temperature.
Cognitive difficulties, often referred to as “brain fog,” can make it hard to concentrate or remember things. Hair loss or thinning, brittle hair, dry skin, and brittle nails are also common, along with unexplained weight gain or difficulty losing weight. Digestive issues, particularly constipation, are frequently reported. Additionally, some people notice puffiness in the face, a slowed heart rate, and musculoskeletal pain, including joint pain, stiffness, muscle aches, weakness, and tenderness. These symptoms can range from subtle to severe, becoming more pronounced as thyroid function continues to decline.
Early Signs and How to Recognize Them
While Hashimoto’s disease can present with several obvious symptoms, there are also more subtle signs that may indicate its onset. These early signs include:
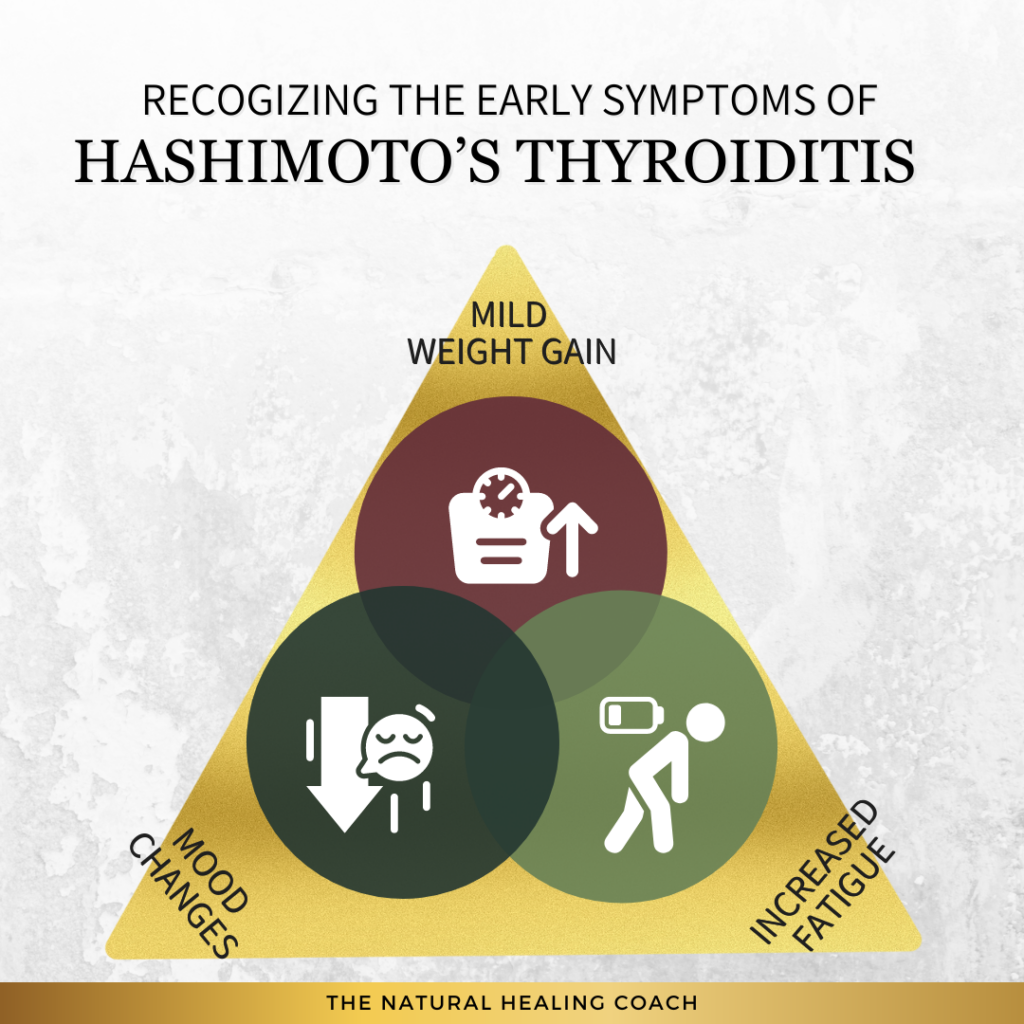
- Mild Weight Gain: Unexplained, gradual weight gain.
- Slight Increases in Fatigue: Noticeable but manageable increases in tiredness or lack of energy.
- Mood Changes: Early signs may also include mood changes such as increased anxiety or depression.
Recognizing these early symptoms is crucial to seeking a diagnosis and starting treatment before the condition progresses significantly. Early intervention can help manage symptoms more effectively and prevent further complications associated with hypothyroidism.
Causes of Hashimoto’s
Understanding the underlying causes of Hashimoto’s disease can help you gain insight into why the condition develops and how it can be managed. Hashimoto’s is primarily driven by autoimmune dysfunction, but both genetic and environmental factors also play a significant role in its onset.
Autoimmune Triggers Behind Hashimoto’s
As previously mentioned, Hashimoto’s occurs when the immune system, which normally protects the body from harmful invaders, mistakenly targets the thyroid gland. This autoimmune response leads to chronic inflammation and damage to the thyroid tissue, gradually impairing its ability to produce essential hormones. The exact trigger for this autoimmune dysfunction is not fully understood, but it is believed to involve a combination of genetic predisposition and environmental influences.
Genetic and Environmental Influences
While anyone can develop Hashimoto’s disease, certain genetic factors may increase the likelihood of its onset. Individuals with a family history of autoimmune diseases, particularly thyroid disorders, are at a higher risk. Environmental factors, such as chronic stress, exposure to toxins, infections, and dietary deficiencies, can also contribute to the development of Hashimoto’s. These factors may interact with genetic predispositions, triggering the autoimmune response that leads to the disease.
Risk Factors for Hashimoto’s Disease
Recognizing the risk factors associated with Hashimoto’s disease can help you understand who is more likely to develop this condition. While some risk factors are beyond your control, such as genetics and age, others are related to lifestyle choices that can be managed to reduce your risk.
Who is Most at Risk?
Certain populations are more susceptible to developing Hashimoto’s disease. Women are significantly more likely to be diagnosed with Hashimoto’s than men, particularly those between the ages of 30 and 50. Additionally, a family history of thyroid disorders or other autoimmune diseases increases the likelihood of developing Hashimoto’s, as genetic factors play a crucial role in its onset.
Lifestyle Factors That Increase Risk
Certain lifestyle choices can contribute to the development or exacerbation of Hashimoto’s:
- Chronic Stress: Prolonged stress can exacerbate the autoimmune response that leads to Hashimoto’s disease.
- Poor Diet: Diets lacking in essential nutrients, particularly iodine and selenium, can impair thyroid function and contribute to the development of Hashimoto’s.
- Exposure to Environmental Toxins: Regular exposure to harmful substances can increase the risk of triggering autoimmune responses.
- Low Nutrient Intake: Deficiencies in key nutrients like iodine and selenium can negatively affect thyroid health and increase susceptibility to Hashimoto’s.
Managing stress, maintaining a balanced diet, and reducing exposure to harmful substances can help lower your risk.
Diagnosis of Hashimoto’s Disease
Early diagnosis is essential for managing Hashimoto’s disease effectively and preventing long-term complications. The diagnostic process involves several key blood tests that provide a comprehensive picture of thyroid health, helping to confirm the presence of Hashimoto’s and guide appropriate treatment.
Common Diagnostic Tests for Hashimoto’s
Diagnosing Hashimoto’s disease typically involves a series of blood tests that evaluate thyroid function and detect autoimmune activity. Here’s an overview of the key tests commonly used in this process:
Table 1. Hashimoto’s Diagnostic Tests
| Diagnostic Test | Purpose | Description |
|---|---|---|
| Thyroid Stimulating Hormone (TSH) | Assesses thyroid function | Measures the level of TSH in the blood. Elevated TSH levels may indicate that the thyroid is underactive, a hallmark of Hashimoto’s disease. |
| Thyroxine (T4) | Evaluates overall thyroid hormone production | Measures the level of total T4, the primary hormone produced by the thyroid. Low T4 levels can signal hypothyroidism, commonly associated with Hashimoto’s. |
| Free T4 (FT4) | Provides a more accurate measure of active thyroid hormone | Measures the unbound (active) form of T4. Free T4 offers a clearer indication of thyroid function than total T4. |
| Triiodothyronine (T3) | Assesses the active form of thyroid hormone | Measures the level of T3, the active form of thyroid hormone. Low T3 levels may contribute to hypothyroid symptoms, even if T4 levels appear normal. |
| Reverse T3 (rT3) | Identifies issues with hormone conversion | Measures the level of reverse T3, an inactive form of T3. High rT3 levels can suggest that the body is converting T4 into inactive rT3 rather than active T3, leading to hypothyroid symptoms. |
| Anti-Thyroid Peroxidase (anti-TPO) Antibody | Detects autoimmune response against the thyroid gland | Identifies the presence of anti-TPO antibodies, which are often elevated in Hashimoto’s, indicating an autoimmune attack on the thyroid. |
| Anti-Thyroglobulin Antibody (TgAb) | Further assesses autoimmune thyroid activity | Measures antibodies against thyroglobulin, another protein produced by the thyroid. Elevated levels of TgAb can indicate autoimmune thyroid conditions like Hashimoto’s. |
These tests provide a detailed view of thyroid function and autoimmune activity, allowing for a precise diagnosis of Hashimoto’s disease.
Steps to Diagnosing
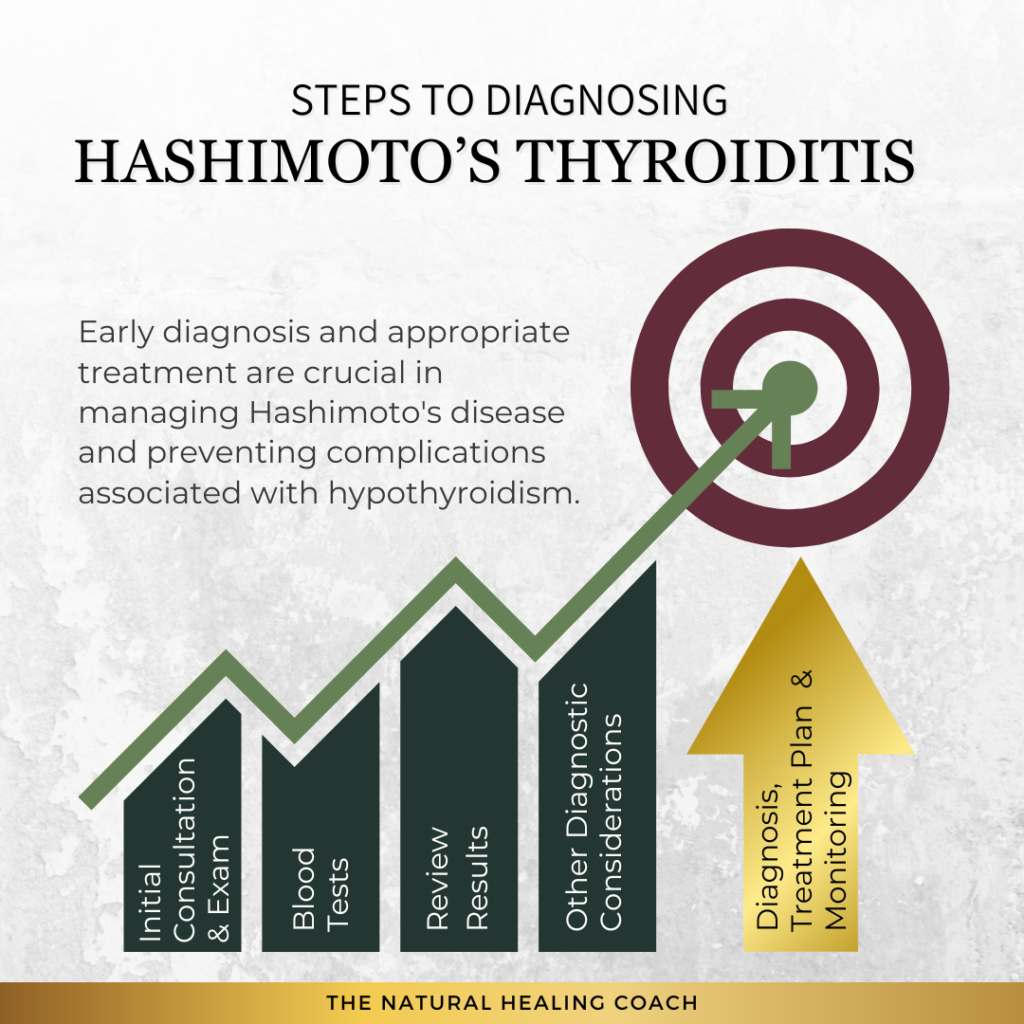
It’s important to seek medical evaluation if you experience persistent symptoms such as fatigue, unexplained weight gain, sensitivity to cold, or other signs of thyroid dysfunction. Individuals with a family history of thyroid disorders or other autoimmune diseases should be especially vigilant. Early intervention can prevent the progression of Hashimoto’s and allow for more effective management. If you notice these symptoms or any other changes in your health, it’s advisable to consult a healthcare professional for a thorough evaluation.
Here are the steps typically involved in diagnosing Hashimoto’s disease:
By following these steps, you can ensure that Hashimoto’s disease is accurately diagnosed and managed effectively, helping you maintain better overall health.
Treatment Options for Hashimoto’s Disease
When managing Hashimoto’s disease, a comprehensive treatment plan often includes a combination of conventional medical treatments and medications tailored to the individual’s needs. While thyroid hormone replacement therapy remains the cornerstone of treatment, other medications and approaches may also be necessary to address specific symptoms and complications.
Conventional Medical Treatments
The standard treatment for Hashimoto’s disease typically involves thyroid hormone replacement therapy, with levothyroxine (Synthroid, Levoxyl, Euthyrox) being the most commonly prescribed medication. This synthetic form of the T4 hormone helps restore normal thyroid levels, alleviating symptoms like fatigue, weight gain, and cold intolerance. Regular monitoring and adjusting the dosage based on blood test results are crucial to maintaining optimal thyroid function.
For some patients, liothyronine (Cytomel), a synthetic T3 hormone, may be prescribed alongside levothyroxine, especially if the body struggles to convert T4 to T3. Additionally, desiccated thyroid extracts (such as Armour Thyroid, Nature-Thyroid, or WP Thyroid) offer a natural alternative, combining both T4 and T3 hormones, although they are less commonly used and require careful dosing due to variability in hormone content.
Table 2. Common Conventional Hashimoto’s Medications
| Treatment | Pros | Cons |
|---|---|---|
| Levothyroxine (Synthroid, Levoxyl, Euthyrox) | – Widely used and well-tolerated. | – Requires regular monitoring and dose adjustments. |
| – Restores normal thyroid levels effectively. | – May not fully alleviate symptoms for all patients. | |
| Liothyronine (Cytomel) | – Directly increases active thyroid hormone levels. | – Can cause symptoms of hyperthyroidism if not properly dosed. |
| – Useful for patients who have difficulty converting T4 to T3. | – Requires more frequent dosing than T4. | |
| Desiccated Thyroid Extracts (Armour Thyroid, Nature-Throid, WP Thyroid) | – Provides a combination of T4 and T3 hormones. | – Variable hormone content can lead to inconsistent dosing. |
| – Some patients prefer natural alternatives. | – Not as widely recommended by conventional doctors. |
Other Medications for Hashimoto’s Disease
Beyond hormone replacement, several other medications may be part of the treatment plan:
Table 3. Other Common Hashimoto’s Medications
| Medication | Pros | Cons |
|---|---|---|
| Beta-Blockers | – Effective for controlling heart rate and anxiety. | – Only addresses symptoms, not the underlying condition. |
| NSAIDs | – Reduces inflammation and pain. | – Long-term use can lead to gastrointestinal issues. |
| Corticosteroids | – Powerful anti-inflammatory effects. | – Significant side effects with long-term use (e.g., weight gain, bone thinning). |
| Immunosuppressants | – Reduces immune system activity in severe cases. | – Increases risk of infections and other side effects. |
| Cholesterol-Lowering Medications | – Helps manage high cholesterol associated with hypothyroidism. | – May require long-term use with potential side effects. |
| Calcium and Vitamin D Supplements | – Supports bone health, especially important for those at risk of osteoporosis. | – Overuse can lead to kidney stones or other complications. |
Complementary and Alternative Therapies
In addition to conventional treatments, many individuals with Hashimoto’s disease explore complementary and alternative therapies to further support their health. Dietary changes, such as adopting an autoimmune protocol (AIP) or gluten-free diet, can reduce inflammation and support thyroid function. Supplements like selenium and zinc, which play a role in thyroid health, may also be beneficial.
Integrative approaches, including stress management techniques, acupuncture, and herbal remedies, can enhance overall well-being and help manage Hashimoto’s symptoms more effectively. Combining these therapies with conventional treatments offers a holistic approach to managing the disease, addressing both the physical and emotional aspects of living with Hashimoto’s.
Table 4. Complementary and Alternative Therapies
| Therapy | Pros | Cons |
|---|---|---|
| Dietary Changes (AIP, Gluten-Free) | – Can reduce inflammation and improve overall health. | – Requires significant lifestyle changes and commitment. |
| Nutritional Supplements (Selenium, Zinc) | – Supports thyroid function and overall immune health. | – May not be effective for everyone and requires proper dosing. |
| Acupuncture | – Can help reduce stress and improve well-being. | – Results can vary; not a cure for thyroid dysfunction. |
| Herbal Remedies | – Offers natural options for symptom management. | – Limited scientific evidence; potential interactions with medications. |
| Stress Management Techniques | – Improves mental health and may reduce autoimmune flare-ups. | – Requires consistent practice and may not directly affect thyroid levels. |
Combining these therapies with conventional treatments offers a holistic approach to managing the disease, addressing both the physical and emotional aspects of living with Hashimoto’s.
Managing Hashimoto’s disease involves a multifaceted approach that includes not only thyroid hormone replacement therapy but also a range of other medications and lifestyle modifications tailored to the individual’s needs. By working closely with healthcare providers, patients can achieve better symptom control and maintain a higher quality of life.
Living with and Flare Management for Hashimoto’s Disease
Managing Hashimoto’s disease is a lifelong journey that requires both adherence to treatment plans and continuous adjustments in daily life. By following specific strategies, you can maintain your well-being and effectively handle flare-ups when they occur.
Daily Management Tips
Maintain a Balanced Diet: Focus on a nutrient-dense diet that supports thyroid function and reduces inflammation.
- Incorporate foods rich in selenium (e.g., Brazil nuts, tuna), zinc (e.g., pumpkin seeds, chickpeas), and iodine (if not contraindicated).
- Consider an autoimmune protocol (AIP) or gluten-free diet if recommended by your healthcare provider.
Engage in Regular Physical Activity: Regular exercise can boost energy levels, support metabolic function, and reduce stress.
- Participate in moderate activities like walking, swimming, yoga, or strength training.
- Listen to your body and avoid overexertion.
Practice Stress Management: Chronic stress can worsen Hashimoto’s symptoms, so it’s important to incorporate stress-reducing practices into your routine.
- Try mindfulness meditation or deep breathing exercises daily.
- Spend time in nature or engage in hobbies that help you relax.
Establish a Consistent Sleep Routine: Quality sleep is essential for hormone regulation and overall health.
- Aim for 7-9 hours of sleep each night.
- Create a calming bedtime routine and maintain a regular sleep schedule.
Adhere to Medication Schedules: Consistently taking your thyroid medication as prescribed is crucial for managing Hashimoto’s.
- Take your medication at the same time each day, ideally on an empty stomach.
- Schedule regular check-ups with your healthcare provider to monitor and adjust your dosage as needed
Monitor Your Symptoms: Keeping track of your symptoms can help identify patterns and triggers, aiding in more effective management.
- Use a symptom diary or a tracking app to log changes in your health.
- Discuss these observations with your healthcare provider to refine your treatment plan.
Strategies for Managing Flares
Consult Your Healthcare Provider: If you experience worsening symptoms, it may be necessary to adjust your medication temporarily.
- Contact your doctor to discuss your symptoms and potential medication adjustments.
- Follow up with blood tests if recommended to ensure proper hormone levels.
Increase Rest and Relaxation: During a flare, your body needs extra rest to recover.
- Allow for more sleep and take short naps during the day if needed.
- Reduce your overall stress load by postponing non-essential tasks or activities.
Modify Your Diet: Adjusting your diet during a flare can help reduce inflammation.
- Eliminate potential trigger foods such as gluten, dairy, or sugar. Focus on anti-inflammatory foods like leafy greens, fatty fish, and turmeric.
Stay Hydrated and Support Nutrient Intake: Proper hydration and nutrient support can aid in managing a flare.
- Drink plenty of water throughout the day.
- Consider supplements like selenium, magnesium, and omega-3 fatty acids under your doctor’s guidance.
Intensify Stress Management: During a flare, stress management becomes even more critical.
- Engage in gentle yoga or meditation more frequently.
- Take short, mindful walks to help calm your nervous system.
Communicate with Your Support System: Let your family, friends, or colleagues know that you’re experiencing a flare.
- Explain your current condition so they can offer support or adjust expectations.
- Don’t hesitate to ask for help with tasks or responsibilities.
Stay in Touch with Your Healthcare Team: Keeping close contact with your healthcare provider during a flare can provide additional support and guidance.
- Schedule a check-up or telehealth visit if symptoms persist.
- Follow your provider’s recommendations for additional treatments or interventions during the flare.
By following these numbered strategies and implementing the example tips, you can better manage daily life with Hashimoto’s disease and effectively reduce the impact of flares. This approach empowers you to take control of your health and maintain your well-being despite the challenges posed by the condition.
Importance of Support Systems and Mental Health Management
Living with Hashimoto’s disease can be challenging, affecting both your physical and emotional well-being. Building strong support systems and effectively managing your mental health are essential components of a comprehensive approach to living well with this condition.
Support Systems
- Join Hashimoto’s Support Groups: Connecting with others who have Hashimoto’s can offer invaluable emotional support, understanding, and practical tips for managing the disease. Consider joining local or online support groups where you can share experiences and advice.
- Educate and Communicate with Loved Ones: It’s important to help your family and friends understand Hashimoto’s disease so they can offer better support. Open communication about your condition can foster empathy and encourage your loved ones to be more supportive in your health journey.
Mental Health Management
- Seek Professional Help: If Hashimoto’s is affecting your mental health, consider consulting a mental health professional. Therapy can provide you with tools and strategies to cope with the emotional challenges of living with a chronic illness, such as anxiety or depression.
- Practice Personalized Stress Management: Tailor stress management techniques to fit your lifestyle and specific triggers. While general stress management is important, consider activities like mindfulness meditation, gentle yoga, or nature walks, which can be particularly beneficial in managing the unique stressors associated with Hashimoto’s disease.
By incorporating daily management tips, flare management strategies, and prioritizing support systems and mental health, individuals with Hashimoto’s disease can enhance their quality of life and gain better control over their condition. Collaborating closely with healthcare providers to customize these approaches to individual needs is crucial for effective management.
Myths and Facts About Hashimoto’s Disease
Misconceptions about Hashimoto’s disease are common and can lead to confusion and misinformation. Understanding the facts is crucial for managing the condition effectively and dispelling any myths that may hinder proper treatment.
Common Misconceptions About Hashimoto’s
Here are some widespread myths about Hashimoto’s disease, along with the facts to clarify these misconceptions:
Myth 1: Hashimoto’s Disease Only Affects Older Women
While Hashimoto’s is more common in women, it can affect people of all ages and genders, including men and younger individuals. It’s important for anyone experiencing symptoms to seek medical evaluation, regardless of age or gender.
Myth 2: Hashimoto’s Can Be Cured with Diet Alone
While diet and lifestyle changes can play a significant role in managing symptoms and improving overall health, Hashimoto’s disease cannot be cured by diet alone. It is a chronic autoimmune condition that typically requires ongoing medical treatment, such as thyroid hormone replacement therapy.
Myth 3: Symptoms Will Always Improve Quickly with Treatment
The effectiveness of treatment can vary from person to person, and it may take time to find the right dosage of thyroid hormone replacement or the right combination of treatments. Patience and regular monitoring by a healthcare provider are key to managing the disease effectively.
Myth 4: You Can’t Live a Normal Life with Hashimoto’s Disease
With proper management, many people with Hashimoto’s disease live healthy, active lives. While it may require adjustments to lifestyle and ongoing treatment, Hashimoto’s can be effectively managed, allowing individuals to maintain a good quality of life.
Myth 5: Hashimoto’s Disease Always Leads to Severe Hypothyroidism
While Hashimoto’s is a leading cause of hypothyroidism, not everyone with Hashimoto’s will experience severe symptoms. Early diagnosis and treatment can help prevent the progression of the disease and manage symptoms effectively.
The Truth About Hashimoto’s and Weight Loss
One of the most persistent misconceptions about Hashimoto’s disease is related to weight loss. Many believe that weight gain is inevitable with Hashimoto’s and that losing weight is nearly impossible. Here’s the truth:
Myth 6: Weight Gain is Unavoidable and Losing Weight is Impossible with Hashimoto’s Disease
While Hashimoto’s can slow metabolism and contribute to weight gain, it is not impossible to manage your weight with this condition. Proper treatment, including thyroid hormone replacement, combined with a balanced diet and regular physical activity, can help manage weight. It may require more effort and patience, but weight loss is achievable with the right approach and support.
Myth 7: All Weight Gain with Hashimoto’s is Due to Hypothyroidism
While hypothyroidism associated with Hashimoto’s can slow metabolism and lead to weight gain, not all weight gain is directly related to thyroid dysfunction. Other factors, such as diet, lifestyle, stress, and coexisting conditions, can also contribute to weight changes. It’s important to consider the whole picture when addressing weight management with Hashimoto’s.
Myth 8: Once You Start Thyroid Medication, You’ll Automatically Lose Weight
While thyroid hormone replacement can help normalize metabolism, it doesn’t guarantee weight loss. Weight loss with Hashimoto’s often requires a combination of proper medication management, a balanced diet, and regular physical activity. Some people may experience a reduction in symptoms like fatigue and water retention, but sustained weight loss usually requires a comprehensive approach.
Myth 9: You Should Drastically Cut Calories to Lose Weight with Hashimoto’s
Severely restricting calories can actually be counterproductive for those with Hashimoto’s disease. Extreme calorie restriction can further slow metabolism and lead to nutrient deficiencies, which can worsen symptoms. A balanced, nutrient-dense diet with appropriate portion sizes is more effective for weight management and overall health.
Myth 10: You Can’t Build Muscle or Improve Fitness with Hashimoto’s
People with Hashimoto’s can still build muscle and improve their fitness levels. While hypothyroidism can make it more challenging due to fatigue and slower recovery times, a consistent exercise routine, including strength training and cardio, can improve metabolism, muscle mass, and overall energy levels. Adjustments to intensity and recovery times may be needed, but fitness goals are achievable.
Myth 11: All Weight Gain with Hashimoto’s is Permanent
Weight gained due to Hashimoto’s is not necessarily permanent. With the right treatment and lifestyle changes, it’s possible to lose the weight gained during periods of hypothyroidism. It’s important to approach weight loss with patience, as it may take time to see results, but it is possible with consistent effort.
These myths can create unnecessary anxiety or lead to ineffective strategies for managing weight with Hashimoto’s disease. Understanding the facts can help individuals approach their health and weight management more effectively and with greater confidence.
By understanding these myths and the facts behind them, individuals with Hashimoto’s disease can better navigate their condition, seek appropriate treatment, and maintain a positive outlook on their health and well-being.
Support and Resources for Hashimoto’s
Finding support and accessing reliable resources can make a significant difference in managing psoriasis. Here are some organizations, support groups, online communities, and educational resources for individuals with psoriasis:
Organizations
- American Thyroid Association (ATA):
- Provides comprehensive information on thyroid disorders, research updates, and resources for patients and healthcare providers.
- Thyroid.org
- Thyroid Foundation of Canada:
- Offers support, education, and awareness for thyroid patients and their families.
- Thyroid Foundation of Canada
Online Communities and Forums
Educational Resources
- American Thyroid Association (ATA):
- Extensive information on thyroid disorders, including Hashimoto’s, with patient guides, research updates, and treatment options.
- www.thyroid.org
- Thyroid Federation International:
- A global network of patient organizations providing support, education, and advocacy for thyroid patients.
- www.thyroid-fed.org
Podcasts
- The Thyroid Fixer Podcast:
- Hosted by Dr. Amie Hornaman, this podcast covers all things thyroid-related, including Hashimoto’s, and offers practical advice on managing thyroid health.
Podcast – Dr. Amie (dramie.com)
- Hosted by Dr. Amie Hornaman, this podcast covers all things thyroid-related, including Hashimoto’s, and offers practical advice on managing thyroid health.
- Help for Hashimoto’s Podcast:
- Offers insights into living with Hashimoto’s disease, including tips on diet, lifestyle, and managing symptoms.
- www.helpforhashimotos.com/podcast
Final Thoughts
Living with Hashimoto’s disease is a journey that can be filled with challenges, but it also offers opportunities for growth and self-discovery. Over the years, I’ve come to realize that managing this condition goes beyond just medical treatments—it’s about embracing a holistic approach that nurtures both the body and the mind. This journey has taught me the importance of listening to my body, seeking knowledge, and finding balance in all aspects of life.
I want to encourage you to take charge of your health with confidence and hope. Every small step you take towards understanding and managing Hashimoto’s can make a significant difference in your well-being. Whether it’s adjusting your diet, finding stress-relief techniques that work for you, or connecting with others who share your experiences, know that you have the power to improve your quality of life. Remember, you’re not alone in this journey—there are countless resources, communities, and healthcare professionals ready to support you.
The broader implications of managing Hashimoto’s disease effectively extend far beyond just symptom relief. By actively participating in your health management, you’re setting the foundation for a healthier, more fulfilling life. You’re also contributing to a greater understanding of this condition within your community, helping to raise awareness and support for others who might be facing similar challenges.
I encourage you to continue exploring this topic and seeking out new ways to enhance your well-being. The knowledge and strategies you gain along the way will not only benefit you but also empower others as you share your experiences. Whether it’s diving deeper into the latest research, trying out new therapies, or simply staying connected with supportive communities, your journey with Hashimoto’s is a path of ongoing discovery.
As we look to the future, I see a world where Hashimoto’s disease is better understood, more effectively managed, and where those affected by it can live vibrant, healthy lives. Advances in medical science, combined with our collective efforts to educate and support one another, will continue to improve the lives of those with Hashimoto’s. Stay hopeful, stay engaged, and remember that your health journey is a powerful story of resilience and empowerment.
Call to Action
If you found this information helpful and want to learn more about managing autoimmune conditions and staying active, we invite you to engage with our community. Join the conversation, share your experiences, and connect with others who are on the same journey towards better health.
Stay Informed and Connected
- Engage on Social Media: Follow us on your favorite social media platforms for daily tips, inspiration, and community support. We regularly share practical advice, uplifting stories, and the latest research on exercising with autoimmune conditions. Join the conversation and be part of a supportive community.
Subscribe to Our Newsletter
- Exclusive Insights: Get in-depth articles and updates on the latest research in autoimmune health directly to your inbox.
- Health Tips: Receive practical tips and strategies for managing your condition and improving your overall well-being.
- Stay Updated: Be the first to know about new blog posts, upcoming events, and other valuable resources.
Join the Discussion
- Leave a Comment: We’d love to hear your thoughts and experiences. Share your insights in the comments below and connect with others who are on the same journey. Your comments help build a supportive community where everyone can learn and grow together.
Together, we can take proactive steps towards better health and well-being, even with autoimmune disease.
If you are looking for more tips and support, join me over on my group page, The Village – A Natural HEALing Community, to get tons of information and tips to help you take your HEALTHY EATING and ACTIVE LIVING to the next level.
REFERENCES:
- American Thyroid Association. “Hashimoto’s Thyroiditis.” Thyroid.org.
- Mayo Clinic. “Hashimoto’s Disease.” MayoClinic.org.
- American Association of Clinical Endocrinologists (AACE). “What Is Hashimoto’s Disease?”
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Hashimoto’s Disease.”
- Endocrine Society. “Hashimoto Disease.”
- Harvard Medical School. “Hypothyroidism: Hashimoto’s Disease.” Harvard Health Publishing. Accessed August 2024.
MORE RELATED POSTS:








+leave a comment . . .