Introduction
Imagine you’re at the gym, going through your usual routine. Recently, things have started to feel different. Despite your regular workouts, you’re more fatigued than usual. Your muscles ache more, and you’ve been experiencing sudden bursts of heat that leave you sweating profusely, even during light exercises. You start to wonder if these changes could be linked to something more significant.
Menopause is a natural biological process that marks the end of a woman’s menstrual cycles. It’s a significant phase in a woman’s life, typically occurring in the late 40s to early 50s. Perimenopause, on the other hand, is the transitional period leading up to menopause, which can start as early as the mid-30s and last for several years. During this time, women may experience a variety of symptoms that can signal the approach of menopause.
Recognizing the signs of menopause and perimenopause is crucial for managing the associated symptoms and maintaining overall health and well-being. Understanding these signs can help you prepare for and navigate this transition more smoothly, ensuring that you can take proactive steps to support your body during this time.
One of the key factors influencing these changes is the fluctuation and eventual decline of hormone levels, particularly estrogen and progesterone.
One sign on the wall of my doctor’s office that always resonated with me was the quote: “We age because our hormones decline. Our hormones don’t decline because we age.” This statement highlights the profound impact that hormones have on our aging process and underscores the importance of maintaining hormonal balance. It suggests that by understanding and managing our hormone levels, we can potentially decelerate the aging process and improve our quality of life during menopause and beyond. We will dig deeper into this quote later in the blog.
But for now, to fully grasp the changes and symptoms you’re experiencing, it’s important to understand what menopause and perimenopause entail. Let’s delve into the definitions and differences between these two phases, and how they impact your body and health.
Understanding Menopause and Perimenopause
Definition of Menopause
Menopause is a natural biological process that signifies the end of a woman’s menstrual cycles. It is officially diagnosed after a woman has gone 12 consecutive months without a menstrual period. This phase typically occurs in women in their late 40s to early 50s, although it can happen earlier or later for some. Menopause marks the end of a woman’s reproductive years and the cessation of ovarian function. During menopause, the body undergoes significant hormonal changes, particularly a decrease in the production of estrogen and progesterone.
These hormonal shifts can lead to a variety of physical and emotional symptoms, making it a pivotal time in a woman's life that requires understanding and management. Share on XDefinition of Perimenopause
Perimenopause, often referred to as the transition to menopause, is the period leading up to menopause. It is characterized by various physical and hormonal changes as the body gradually transitions from regular menstrual cycles to complete cessation. Perimenopause can begin as early as a woman’s 30s or 40s and can last anywhere from a few years to over a decade.
Understanding perimenopause is crucial for several reasons:
- First, it helps women recognize that the changes they are experiencing are normal and part of a natural process.
- Second, it allows women to seek appropriate medical advice and support to manage symptoms effectively. Awareness and education about perimenopause can also help in making lifestyle adjustments that can ease the transition.
By understanding the early signs and symptoms of perimenopause, women can take proactive steps to support their health and well-being during this transitional phase.
Racial and Ethnic Differences in Perimenopause and Menopause: A Closer Look at BIPOC and White Women’s Experiences
Building on the understanding that perimenopause and menopause are natural biological processes experienced by all women, it’s important to recognize that these stages can manifest differently across various racial and ethnic groups, including BIPOC (Black, Indigenous, and People of Color) and white women.
Below are key statistics and findings that highlight these differences:
Age of Onset
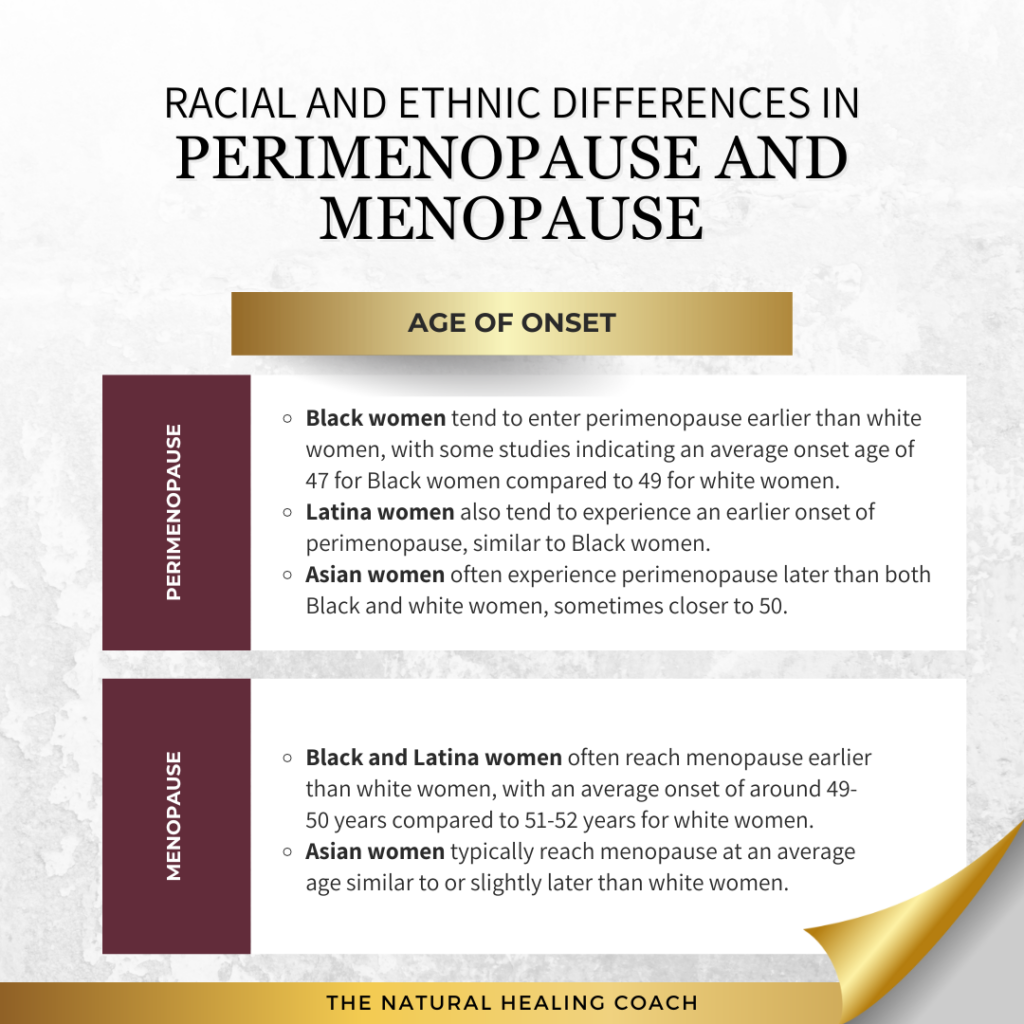
- Perimenopause:
- Black women tend to enter perimenopause earlier than white women, with some studies indicating an average onset age of 47 for Black women compared to 49 for white women.
- Latina women also tend to experience an earlier onset of perimenopause, similar to Black women.
- Asian women often experience perimenopause later than both Black and white women, sometimes closer to 50.
- Menopause:
- Black and Latina women often reach menopause earlier than white women, with an average onset of around 49-50 years compared to 51-52 years for white women.
- Asian women typically reach menopause at an average age similar to or slightly later than white women.
Symptom Severity and Duration
- Symptom Severity:
- Black women tend to report more severe vasomotor symptoms (hot flashes, night sweats) compared to white women.
- Latina women also report higher levels of symptom severity, particularly with mood changes and sleep disturbances.
- Asian women generally report fewer and less severe vasomotor symptoms compared to both Black and white women.
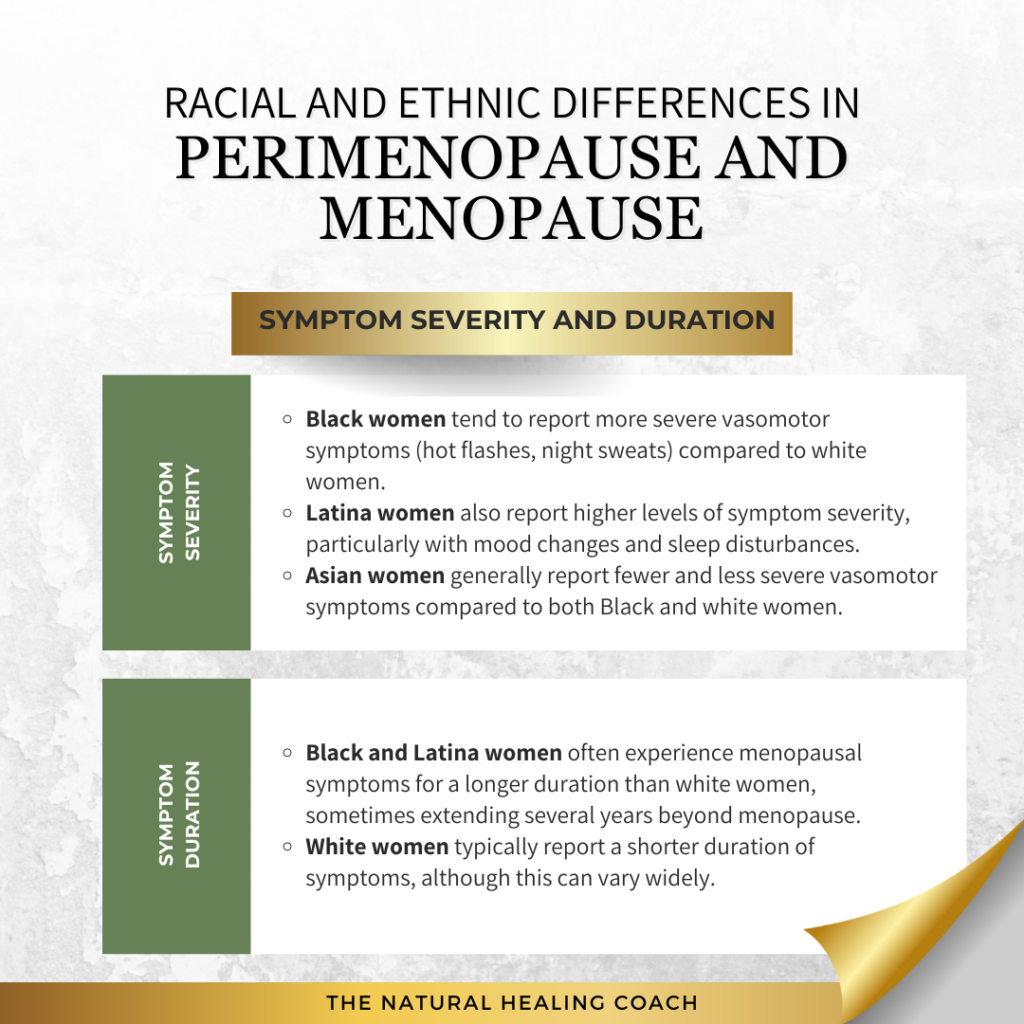
- Symptom Duration:
- Black and Latina women often experience menopausal symptoms for a longer duration than white women, sometimes extending several years beyond menopause.
- White women typically report a shorter duration of symptoms, although this can vary widely.
Health Outcomes and Risks
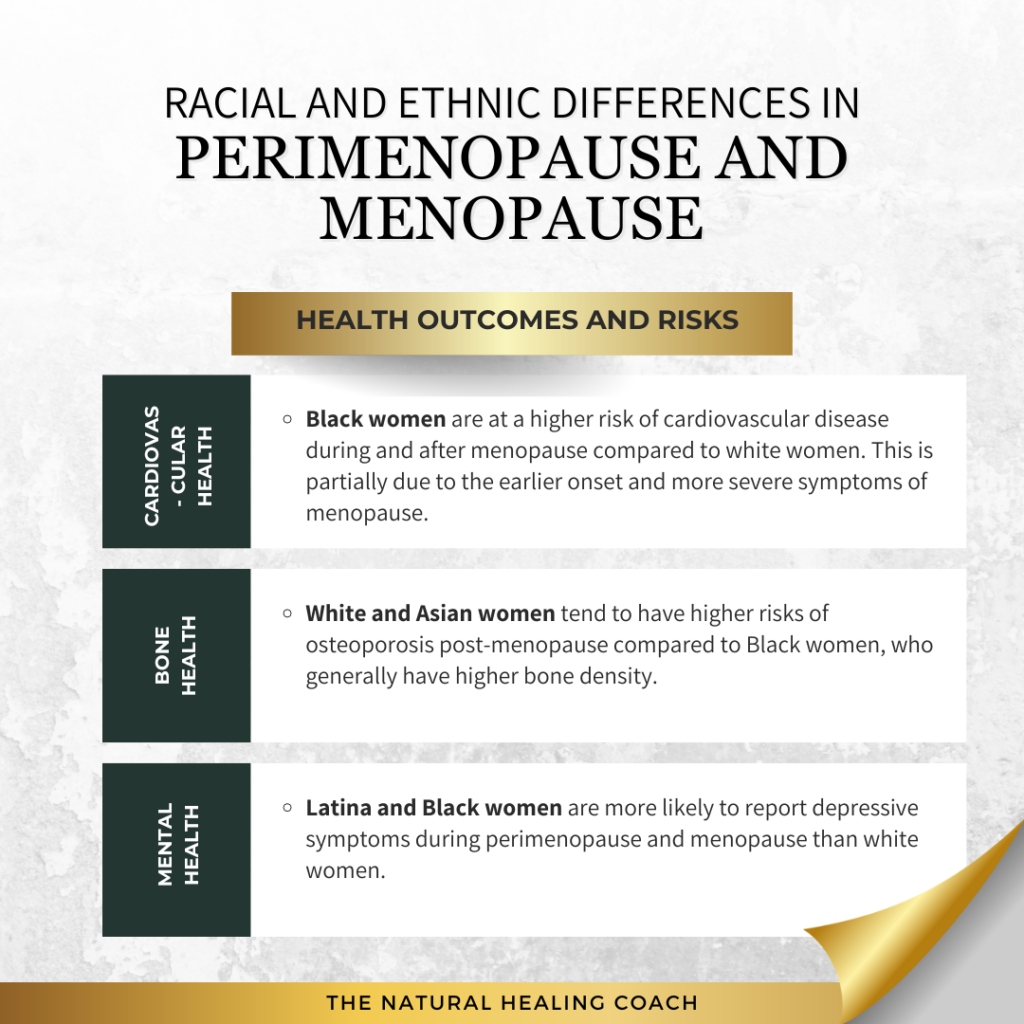
- Cardiovascular Health:
- Black women are at a higher risk of cardiovascular disease during and after menopause compared to white women. This is partially due to the earlier onset and more severe symptoms of menopause.
- Bone Health:
- White and Asian women tend to have higher risks of osteoporosis post-menopause compared to Black women, who generally have higher bone density.
- Mental Health:
- Latina and Black women are more likely to report depressive symptoms during perimenopause and menopause than white women.
Access to Care and Cultural Perceptions
- Access to Care:
- BIPOC women often have less access to healthcare services and support for managing perimenopause and menopause symptoms compared to white women. This disparity can lead to untreated symptoms and worse overall health outcomes.
- Cultural Perceptions:
- Cultural attitudes towards menopause can vary significantly. For example, some studies have found that Black and Latina women may have more positive perceptions of menopause compared to white women, viewing it as a natural life transition rather than a medical condition.
These insights underscore the importance of culturally competent care and the need for tailored health education and interventions that address the unique needs of BIPOC women during perimenopause and menopause. Understanding these differences is crucial as we explore the common symptoms experienced during these life stages.
Common Symptoms of Perimenopause and Menopause
Both perimenopause and menopause bring about a variety of symptoms as the body undergoes significant hormonal changes. While there is some overlap, the severity and specific nature of symptoms can differ between these phases. Understanding these differences can help in managing and addressing the symptoms more effectively.
Chart: Differences in Symptoms Between Perimenopause and Menopause
| Symptom | Perimenopause | Menopause |
|---|---|---|
| Irregular Periods | Changes in frequency, duration, and flow | Complete cessation for 12 consecutive months |
| Hot Flashes and Night Sweats | Sudden, frequent warmth | Variable intensity and frequency |
| Sleep Problems | Insomnia, frequent waking | Persistent disturbances, night sweats |
| Mood Changes | Irritability, anxiety, depression | Continued mood swings, influenced by other factors |
| Weight Gain and Metabolism | Gradual weight gain, slowed metabolism | Pronounced weight gain, especially abdominal |
| Thinning Hair and Dry Skin | Initial changes in hair and skin | More noticeable and persistent |
| Loss of Breast Fullness | Gradual changes | Significant loss and texture changes |
| Decreased Libido | Lowered interest in sexual activity | Persistent decreased libido |
| Vaginal Dryness and Discomfort | Some dryness and discomfort | More pronounced and persistent |
| Memory and Concentration | Initial cognitive changes | Continued memory problems, concentration issues |
Recognizing the early symptoms of perimenopause is crucial for timely intervention, improving quality of life, and making informed decisions about treatment. Early awareness allows for lifestyle adjustments, better communication with healthcare providers, and emotional preparedness, all of which contribute to a smoother transition through this stage. Understanding these signs can make a significant difference in managing the journey effectively. Now, let’s delve into the 12 subtle signs of perimenopause you should be aware of.
The 12 Subtle Signs of Perimenopause
While many symptoms of perimenopause are well-known, such as hot flashes and irregular periods, there are several less noticeable signs that someone may be entering this transitional phase. Share on XBeing aware of these subtle symptoms can help women recognize and address perimenopause early on.
- Explanation: Hormonal fluctuations can lead to changes in body odor. Some women may notice that they sweat more or that their sweat smells different.
- Explanation: As estrogen levels drop, the urinary tract can become more sensitive, leading to an increased need to urinate or occasional incontinence.
- Explanation: Hormonal changes can affect the joints and muscles, leading to unexplained aches and pains, stiffness, or soreness.
- Explanation: A subtle decrease in sexual desire can occur, even if vaginal dryness or discomfort isn’t yet present.
- Explanation: Hormonal fluctuations can cause breast tissue to become more sensitive or tender, similar to premenstrual symptoms but potentially more frequent.
- Explanation: Some women may experience occasional heart palpitations or a feeling of the heart beating irregularly, which can be alarming but is often related to hormonal changes.
- Explanation: Reduced estrogen levels can affect the moisture levels in the eyes, leading to dryness and potential changes in vision.
- Explanation: Hormonal fluctuations can impact the digestive system, leading to symptoms such as bloating, gas, or changes in bowel habits.
- Explanation: Skin may become drier, thinner, or more prone to acne and other blemishes due to hormonal shifts.
- Explanation: Hormonal changes can trigger headaches or migraines, even in women who may not have experienced them frequently before.
- Explanation: Some women report a sensation of tingling or numbness in their hands and feet, which can be a result of fluctuating hormone levels.
- Explanation: Hormonal changes can affect the immune system, potentially leading to increased sensitivity to allergies or new allergic reactions.
Recognizing these subtle signs can alert women to the onset of perimenopause, prompting them to seek appropriate guidance from healthcare professionals. Early recognition not only helps manage symptoms but also paves the way for a smoother transition. Understanding these changes is particularly important when considering the connection between perimenopause, hormonal shifts, and autoimmune disease.
The Connection Between Perimenopause, Menopause, Hormones and Autoimmune Disease
As we know, perimenopause and menopause are critical phases in a woman’s life, marked by significant hormonal changes that affect various bodily functions. These hormonal shifts can also have a profound impact on autoimmune diseases, potentially intensifying symptoms or altering the progression of these conditions. Recognizing the interplay between these transitions and autoimmune disease is essential for effective management.
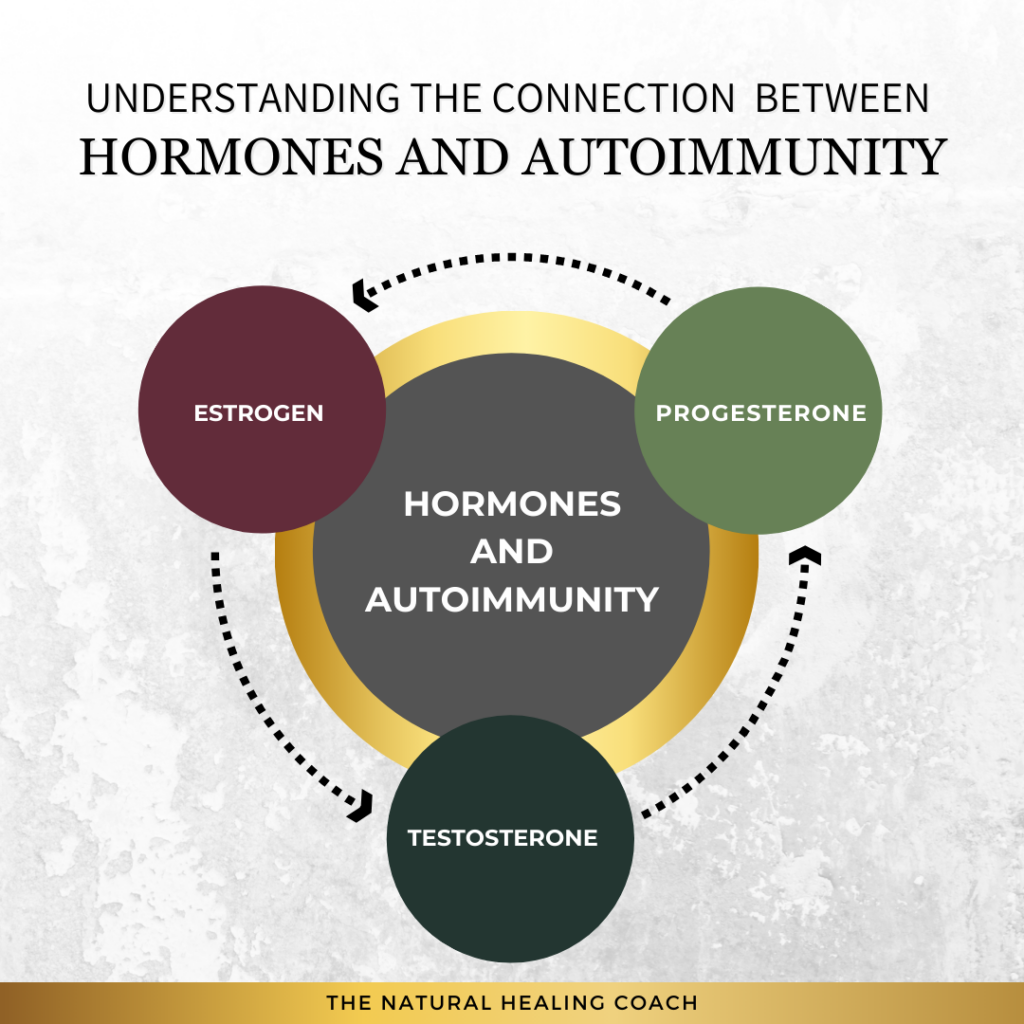
Hormonal Fluctuations and the Immune System
Estrogen and Progesterone
- Role in Immune Function: Estrogen and progesterone are key regulators of the immune system. Estrogen typically enhances immune responses, increasing the activity of immune cells such as T cells and B cells that protect against infections. In contrast, progesterone tends to suppress the immune response, maintaining immune tolerance and preventing the body from attacking its own tissues, particularly during pregnancy.
- Impact of Decline: As women transition through perimenopause and menopause, levels of estrogen and progesterone decrease. This decline can disrupt immune regulation. Reduced estrogen can weaken the body’s defense mechanisms, increasing susceptibility to infections and potentially aggravating autoimmune conditions. Meanwhile, lower progesterone levels can diminish the body’s ability to control immune responses, leading to heightened inflammation and a greater risk of autoimmune disease.
Testosterone
- Role in Immune Function: Although testosterone is often associated with male health, it also plays a vital role in regulating the immune system in women. Testosterone generally suppresses immune activity, helping to prevent an overactive immune response that could lead to autoimmune disorders.
- Impact of Decline: During menopause, testosterone levels also drop, which can reduce the immune system’s regulation. This decrease may lead to an overactive immune response, increasing the likelihood of autoimmune disease flare-ups or the onset of new autoimmune conditions.
Understanding the effects of these hormonal fluctuations on the immune system is crucial for women navigating perimenopause and menopause, especially those with existing autoimmune conditions. By staying informed and proactive, women can work with their healthcare providers to manage these changes and maintain their overall health.
Autoimmune Disease Flare-Ups
Autoimmune Disease Flare-Ups and Hormonal Connections
Hormonal changes during perimenopause and menopause can significantly impact those with autoimmune disease because they often lead to more intense and frequent flare-ups. The decline in key hormones—particularly estrogen, progesterone, and testosterone—can exacerbate symptoms across a range of autoimmune conditions due to their roles in regulating immune function, inflammation, and overall body homeostasis. Here’s how these hormonal changes affect some common autoimmune conditions:
1. Rheumatoid Arthritis (RA)
- Hormones Impacted: Estrogen, Progesterone
- Impact: Estrogen and progesterone have anti-inflammatory properties that help manage joint pain and swelling in RA. As these hormones decline during menopause, the loss of their protective effects can lead to increased inflammation, resulting in more severe and frequent joint pain and stiffness.
2. Systemic Lupus Erythematosus (SLE)
- Hormones Impacted: Estrogen, Progesterone
- Impact: Estrogen plays a significant role in immune system modulation. Its decline during menopause can lead to heightened immune activity, exacerbating lupus symptoms and increasing the frequency and severity of flare-ups. The reduction in progesterone, which also helps regulate immune responses, can further aggravate lupus.
3. Multiple Sclerosis (MS)
- Hormones Impacted: Estrogen, Progesterone
- Impact: Estrogen and progesterone provide protective effects on the central nervous system, which can help manage MS symptoms. The decline in these hormones during menopause may lead to a worsening of neurological symptoms, such as muscle weakness, coordination issues, and fatigue, resulting in more frequent and severe disease activity.
4. Hashimoto’s Thyroiditis
- Hormones Impacted: Estrogen, Progesterone
- Impact: The thyroid is particularly sensitive to changes in estrogen and progesterone levels. During menopause, the decline in these hormones can disrupt thyroid hormone balance, worsening symptoms such as fatigue, weight gain, and mood changes associated with Hashimoto’s thyroiditis.
5. Graves’ Disease
- Hormones Impacted: Estrogen, Progesterone
- Impact: In Graves’ disease, which causes hyperthyroidism, the hormonal shifts during menopause can influence thyroid function. The decline in estrogen and progesterone can lead to fluctuations in thyroid hormone levels, potentially worsening hyperthyroid symptoms like anxiety, rapid heartbeat, and weight loss.
6. Psoriasis
- Hormones Impacted: Estrogen, Progesterone, Testosterone
- Impact: Psoriasis is influenced by skin health and immune regulation, both of which are affected by hormonal changes. The decline in estrogen and progesterone, both of which have anti-inflammatory effects, can worsen skin inflammation. Testosterone also plays a role in skin health, and its decline can further exacerbate psoriasis symptoms.
7. Sjogren’s Syndrome
- Hormones Impacted: Estrogen, Progesterone
- Impact: Sjogren’s syndrome affects the glands that produce tears and saliva, leading to dryness. The decline in estrogen and progesterone during menopause can intensify these symptoms, causing increased dryness and discomfort in women with Sjogren’s.
8. Type 1 Diabetes
- Hormones Impacted: Estrogen, Progesterone, Insulin
- Impact: Hormonal changes during menopause can make blood sugar control more challenging for women with Type 1 diabetes. The decline in estrogen and progesterone affects insulin sensitivity, often requiring adjustments in insulin therapy to maintain stable blood sugar levels.
9. Ankylosing Spondylitis
- Hormones Impacted: Estrogen, Testosterone
- Impact: Ankylosing spondylitis, which primarily affects the spine, can be exacerbated by the decline in both estrogen and testosterone during menopause. Estrogen helps regulate inflammation, while testosterone supports bone health. Their reduction can worsen symptoms such as pain, stiffness, and bone deterioration.
10. Inflammatory Bowel Disease (IBD) – Crohn’s Disease and Ulcerative Colitis
- Hormones Impacted: Estrogen, Progesterone
- Impact: Inflammatory bowel diseases like Crohn’s disease and ulcerative colitis can be exacerbated by the hormonal changes during perimenopause and menopause. The decline in estrogen and progesterone may increase inflammation in the gut, leading to more severe symptoms and more frequent flare-ups.
Why These Hormonal Changes Impact Autoimmune Diseases
The decline in hormones during perimenopause and menopause generally leads to more intense and frequent flare-ups across all autoimmune diseases listed. However, specific distinctions arise based on the nature of each disease and the role these hormones play:
- Increased Inflammation:
- Estrogen and Progesterone have anti-inflammatory properties. Their decline removes a natural check on inflammation, leading to increased inflammatory responses, which can trigger more severe and frequent flares in autoimmune diseases.
- Immune System Dysregulation:
- Hormones like estrogen modulate immune activity. When estrogen levels drop, the immune system may become more aggressive, worsening autoimmune conditions where the immune system is already overactive.
- Tissue-Specific Effects:
- Hormonal declines affect different tissues in ways that can exacerbate symptoms. For instance, estrogen helps maintain joint health, impacting conditions like rheumatoid arthritis, while its decline can lead to worsened joint pain. In contrast, testosterone plays a key role in bone health, influencing diseases like ankylosing spondylitis.
- Disease-Specific Triggers:
- Certain autoimmune diseases have unique triggers influenced by hormonal changes. For example, lupus may experience more severe and systemic flare-ups due to estrogen’s role in antibody production, while MS symptoms may worsen as the protective effects of estrogen and progesterone on the nervous system diminish.
- Impact on Metabolism and Blood Sugar:
- Type 1 Diabetes is particularly affected by the interaction between estrogen, progesterone, and insulin. The decline in these hormones can make blood sugar control more challenging, necessitating careful management and adjustment of therapies.
- Bone Health:
- Ankylosing Spondylitis is influenced by both estrogen and testosterone declines, which affect inflammation and bone density, exacerbating symptoms such as pain and stiffness.
Understanding how hormonal changes during perimenopause and menopause affect autoimmune diseases is essential for effective symptom management and improving the quality of life for women during these transitions. By recognizing these connections and working closely with healthcare providers, women can develop personalized strategies to navigate these challenging phases more effectively.
Symptoms Overlap
During perimenopause and menopause, women often experience a range of symptoms that can overlap with those of autoimmune diseases. This overlap can make it challenging to distinguish whether symptoms are due to hormonal changes or underlying autoimmune conditions. Recognizing these shared symptoms is essential for accurate diagnosis and effective management.
Here are some key symptoms that are commonly seen in both menopause and autoimmune diseases:
- Fatigue: Fatigue is a significant and common symptom in both menopause and autoimmune diseases. The hormonal fluctuations during menopause can lead to profound tiredness, similar to the fatigue experienced in many autoimmune conditions, making it difficult to pinpoint the exact cause.
- Mood Changes: Depression, anxiety, and mood swings are frequent in both menopause and autoimmune diseases. These mood disturbances are often linked to the complex interactions between declining hormone levels and the immune system, which can impact neurotransmitter function and emotional well-being.
- Joint Pain: Hormonal changes during menopause can contribute to joint pain, a symptom also prevalent in many autoimmune diseases like rheumatoid arthritis and lupus. This joint pain can be exacerbated by the decline in estrogen, which has anti-inflammatory properties.
Understanding the overlap between these symptoms is crucial for women navigating both menopause and autoimmune conditions. By recognizing these shared signs, women and their healthcare providers can better tailor their approaches to managing symptoms, ensuring a more effective and comprehensive care plan.
“We Age Because Our Hormones Decline. Our Hormones Don’t Decline Because We Age.”
As we delve deeper into the complexities of perimenopause and menopause, it’s important to revisit the quote mentioned earlier: “We age because our hormones decline. Our hormones don’t decline because we age.” This statement provides a profound insight into the role hormones play in the aging process and underscores the importance of maintaining hormonal balance.
What Does That Really Mean?
Understanding the Role of Hormones in the Aging Process Hormones are chemical messengers that regulate various functions in the body, including metabolism, growth, immune function, and reproduction. Key hormones like estrogen, progesterone, and testosterone play crucial roles in maintaining health and vitality. As we age, the levels of these hormones naturally decline, which can lead to various physical and emotional changes associated with aging.
The Bidirectional Relationship Between Hormone Levels and Aging. The relationship between hormone levels and aging is bidirectional. While aging contributes to the decline in hormone production, reduced hormone levels can accelerate the aging process. For example, lower levels of estrogen and progesterone during menopause can lead to symptoms such as hot flashes, mood swings, and bone density loss, which are commonly associated with aging.
The Impact of Hormonal Balance on Overall Health and Well-being. Maintaining hormonal balance is essential for overall health and well-being. Balanced hormones help regulate mood, energy levels, weight, and cognitive function. When hormone levels are optimal, the body can function more efficiently, and the risk of developing age-related diseases decreases.
Importance of Maintaining Hormonal Balance to Decelerate Aging. By understanding and managing hormone levels, it is possible to decelerate the aging process. Hormonal balance can be achieved through various means, including lifestyle modifications, dietary changes, and medical interventions. Ensuring adequate intake of nutrients that support hormone production, engaging in regular physical activity, and managing stress can all contribute to maintaining hormonal health.
Maintaining hormonal balance is not just about addressing symptoms; it’s about promoting long-term health and vitality. By taking proactive steps to manage hormone levels, it is possible to mitigate the effects of aging and improve overall quality of life during perimenopause, menopause, and beyond. This holistic approach to health emphasizes the interconnectedness of hormones and aging, highlighting the importance of maintaining balance for long-term well-being.
Strategies for Balancing Hormones
Balancing hormones is crucial for overall health and well-being, especially during perimenopause and menopause. Here are several strategies that can help maintain hormonal balance:
Healthy Diet
Nutrient-rich foods play a significant role in supporting hormonal balance. Consuming a variety of whole foods, including fruits, vegetables, lean proteins, and healthy fats, can provide the necessary nutrients for optimal hormone production and regulation.
- Tips:
- Incorporate Healthy Fats: Include sources of healthy fats such as avocados, nuts, seeds, and olive oil to support hormone production.
- Eat Plenty of Fiber: Whole grains, legumes, and vegetables can help regulate blood sugar levels and support digestive health, both of which are important for hormone balance.
- Stay Hydrated: Drink plenty of water to support overall bodily functions, including hormone regulation.
Regular Exercise
Physical activity has numerous benefits for hormonal health. Regular exercise can help reduce stress, maintain a healthy weight, and improve mood, all of which contribute to balanced hormones.
- Tips:
- Mix It Up: Incorporate a variety of exercises, including cardiovascular, strength training, and flexibility workouts, to promote overall health.
- Stay Consistent: Aim for at least 30 minutes of moderate exercise most days of the week.
- Listen to Your Body: Adjust your exercise routine based on how you feel, especially during perimenopause and menopause.
Stress Management
Chronic stress can negatively impact hormone levels. Managing stress through relaxation techniques can help maintain hormonal balance.
- Tips:
- Practice Meditation: Spend a few minutes each day in meditation to calm your mind and reduce stress.
- Try Yoga: Yoga combines physical movement with breath control and meditation, which can help lower stress levels.
- Deep Breathing: Practice deep breathing exercises to activate the body’s relaxation response.
Quality Sleep
Good sleep hygiene is essential for hormone regulation. Poor sleep can disrupt hormone production and lead to imbalances.
- Tips:
- Establish a Routine: Go to bed and wake up at the same time every day to regulate your body’s internal clock.
- Create a Relaxing Environment: Make your bedroom conducive to sleep by keeping it dark, quiet, and cool.
- Limit Screen Time: Avoid screens for at least an hour before bed to reduce blue light exposure that can interfere with sleep.
Avoiding Toxins
Exposure to endocrine disruptors can interfere with hormone production and balance. Reducing exposure to these toxins is important for maintaining hormonal health.
- Tips:
- Use Natural Products: Opt for natural or organic personal care and cleaning products that are free from harmful chemicals.
- Be Mindful of Plastics: Avoid using plastic containers for food and drink, especially when heating, as they can leach harmful chemicals.
- Check Labels: Read labels on products to avoid ingredients known to be endocrine disruptors, such as phthalates and parabens.
Supplements and Herbal Remedies
Certain supplements and herbal remedies can support hormonal balance. However, it’s important to consult with a healthcare provider before starting any new supplement regimen.
- Tips:
- Consider Omega-3s: Omega-3 fatty acids found in fish oil supplements can help reduce inflammation and support hormone health.
- Explore Herbal Options: Herbs like maca root, ashwagandha, and evening primrose oil are known to support hormonal balance.
- Stay Informed: Work with a healthcare provider to determine which supplements are right for you and ensure they don’t interact with any medications you’re taking.
Medical Treatments
For some women, medical treatments such as hormone replacement therapy (HRT) may be necessary to manage symptoms and maintain hormonal balance.
Hormone Replacement Therapy (HRT):
- Types of HRT:
- Estrogen Therapy: For women who have had a hysterectomy.
- Combination Therapy: Estrogen and progesterone for women who still have their uterus.
- Benefits: Can reduce menopausal symptoms like hot flashes, night sweats, and vaginal dryness, and improve quality of life.
- Risks: Potential risks include blood clots, stroke, and certain types of cancer. It’s important to discuss these risks with your healthcare provider.
- Non-Hormonal Medications: Options like antidepressants or medications specifically designed to treat hot flashes can also be helpful.
- Tips:
- Discuss Options: Talk to your healthcare provider about the benefits and risks of HRT and other medical treatments.
- Monitor Effects: Regularly check in with your provider to monitor the effects of any medical treatments and make adjustments as needed.
- Stay Informed: Keep up-to-date with the latest research and guidelines regarding medical treatments for hormonal health.
Regular Check-Ups
Regular check-ups with healthcare professionals are crucial for monitoring hormone levels and overall health. These visits can help detect and address any imbalances early.
- Tips:
- Schedule Routine Visits: Make regular appointments with your healthcare provider to monitor your hormone levels and overall health.
- Be Proactive: Discuss any symptoms or concerns you have with your provider to ensure they are addressed promptly.
- Keep Records: Maintain a health journal to track your symptoms and any changes you notice, which can be helpful during your check-ups.
By adopting these strategies, you can support your hormonal health and navigate the transitions of perimenopause and menopause more smoothly.
Resources
Navigating perimenopause and menopause can be challenging, but there are numerous resources available to help you understand and manage this transition. Here are some valuable resources to consider:
Websites
- North American Menopause Society (NAMS)
- Provides up-to-date information and resources on menopause and perimenopause.
- North American Menopause Society (NAMS)
- National Institute on Aging
- Offers educational articles and resources on menopause.
- National Institute on Aging
- Menopause Matters
- A comprehensive resource for menopause-related information and support.
- Menopause Matters
Online Communities and Forums
- Red Hot Mamas
- A supportive community offering information and discussions about menopause.
- Red Hot Mamas
- Menopause Support
- Provides support, information, and a forum for women experiencing menopause.
- Menopause Support
- Black Girls Guide to Menopause
- Created by Omisade Burney-Scott, this guide offers a mix of storytelling, education, and community-building to support Black women during this transitional life stage. It aims to fill the gap in menopause resources that often overlook the cultural, social, and medical nuances of Black women’s experiences.
- Black Girls Guide to Menopause
- Black Menopause and Beyond
- A resource hub or community dedicated to supporting Black women not only through menopause but also through the post-menopausal phase of life. It focuses on providing information, resources, and support that address the specific needs and concerns of Black women during and after menopause.
- Black Menopause and Beyond
- The Black Menopause Collective
- Brings together Black women to discuss, educate, and support one another through the menopause transition. This collective aims to create a safe space where Black women can share their experiences, access culturally relevant information, and advocate for better healthcare resources and support for Black women going through menopause.
- The Black Menopause Collective
- Black Women in Menopause
- A community focused on raising awareness about the unique challenges and experiences that Black women face during menopause. This platform seeks to provide resources, support, and education specifically tailored to the needs of Black women, ensuring that their voices and stories are included in the broader conversation about menopause.
- Black Women in Menopause
Podcasts
- The Menopause Movement
- Hosted by Dr. Michelle Gordon, this podcast covers various aspects of menopause, including health, wellness, and personal stories.
- The Menopause Movement
- The Happy Menopause
- Hosted by nutritionist Jackie Lynch, this podcast offers practical advice and expert interviews on managing menopause symptoms.
- The Happy Menopause
- Menopause Whilst Black
- Hosted by Karen Arthur, the podcast features candid conversations, interviews, and storytelling that explore the intersection of menopause and race.
- Menopause Whilst Black
Apps
- MenoLife
- A comprehensive app that tracks symptoms, provides educational resources, and connects users with a supportive community.
- MenoLife
- Balance
- Created by Dr. Louise Newson, this app helps track menopause symptoms and provides evidence-based information.
- Balance
- Clue
- A period and ovulation tracker that also includes features for tracking menopause symptoms.
- Clue
Healthcare Providers
- Certified Menopause Practitioners
- NAMS offers a directory of certified practitioners who specialize in menopause care.
- Certified Menopause Practitioners
By leveraging these resources, you can gain a better understanding of perimenopause and menopause, learn strategies to manage symptoms, and connect with a supportive community.
Final Thoughts
Recognizing the symptoms of menopause and perimenopause is essential for managing the physical and emotional changes that come with these life transitions. Early identification of these signs allows for timely intervention, which can significantly improve quality of life. Symptoms such as irregular periods, hot flashes, sleep disturbances, and mood changes can be challenging, but understanding them as part of the natural aging process can empower women to take proactive steps in managing their health.
It is crucial to seek medical advice for personalized hormone management strategies. Each woman’s experience with perimenopause and menopause is unique, and a healthcare provider can offer tailored guidance and treatments. Whether it’s through lifestyle changes, natural supplements, or medical treatments like hormone replacement therapy, having a personalized plan can make a significant difference. Regular check-ups and open communication with a healthcare provider are key to navigating this stage of life effectively.
On a personal note, although I am not in perimenopause, I have taken a proactive approach to managing my hormones overall. Understanding the importance of hormonal balance, I see a hormone doctor to monitor my thyroid and low testosterone levels. This proactive management has been instrumental in maintaining my health and well-being. By addressing these hormonal issues early, I have been able to prevent potential complications and ensure that my body functions optimally.
Taking control of your hormonal health is empowering. It involves listening to your body, being informed about the changes it undergoes, and seeking professional advice when necessary. My journey with hormone management has taught me the value of being proactive and attentive to my body’s needs. Whether you are approaching perimenopause, already experiencing its symptoms, or simply want to take a proactive stance on your health, understanding and managing your hormones is a vital part of ensuring long-term well-being.
Recognizing and addressing the symptoms of perimenopause and menopause is a crucial step in managing your health during this transitional phase. By seeking personalized medical advice, making informed lifestyle choices, and being proactive about hormone management, you can navigate this journey with confidence and resilience. Your health is your most valuable asset, and taking steps to maintain hormonal balance can help you lead a healthier, more vibrant life.
Call to Action
If you found this information helpful and want to learn more about managing autoimmune conditions and staying active, we invite you to engage with our community. Join the conversation, share your experiences, and connect with others who are on the same journey towards better health.
Stay Informed and Connected
- Engage on Social Media: Follow us on your favorite social media platforms for daily tips, inspiration, and community support. We regularly share practical advice, uplifting stories, and the latest research on exercising with autoimmune conditions. Join the conversation and be part of a supportive community.
Subscribe to Our Newsletter
- Exclusive Insights: Get in-depth articles and updates on the latest research in autoimmune health directly to your inbox.
- Health Tips: Receive practical tips and strategies for managing your condition and improving your overall well-being.
- Stay Updated: Be the first to know about new blog posts, upcoming events, and other valuable resources.
Join the Discussion
- Leave a Comment: We’d love to hear your thoughts and experiences. Share your insights in the comments below and connect with others who are on the same journey. Your comments help build a supportive community where everyone can learn and grow together.
Together, we can take proactive steps towards better health and well-being, even with autoimmune disease.
If you are looking for more tips and support, join me over on my group page, The Village – A Natural HEALing Community, to get tons of information and tips to help you take your HEALTHY EATING and ACTIVE LIVING to the next level.
REFERENCES:
- Santoro, N. (2016). Perimenopause: From Research to Practice. Journal of Women’s Health (Larchmt), 25(4), 332-339. https://doi.org/10.1089/jwh.2015.5556
- The North American Menopause Society. (n.d.). Five Solutions for Menopause Symptoms. https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/five-solutions-for-menopause-symptoms
- Management of Perimenopausal and Menopausal Symptoms. (2023). BMJ, 382, e072612. https://doi.org/10.1136/bmj-2022-072612
- Delamater, L., & Santoro, N. (2018). Management of the Perimenopause. Clinical Obstetrics and Gynecology, 61(3), 419-432. https://doi.org/10.1097/GRF.0000000000000389
- Harvard Health Publishing. (2022, August 9). Perimenopause: Rocky Road to Menopause. Harvard Women’s Health Watch. Retrieved from https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause
- Silver, N. E. (n.d.). Mood Changes During Perimenopause Are Real. Here’s What to Know. American College of Obstetricians and Gynecologists (ACOG). Retrieved from https://www.acog.org/womens-health/experts-and-stories/the-latest/mood-changes-during-perimenopause-are-real-heres-what-to-know
- The North American Menopause Society. (n.d.). Menopause 101: A Primer for the Perimenopausal. Retrieved from https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal
- Goldman, L. (2022, April 18). Women of Color, Menopause is Different. Oprah Daily. Retrieved from https://www.oprahdaily.com/life/health/a39649768/women-of-color-menopause/
- Levine, B. (2022, January 13). What Experts Want Women of Color to Know About Menopause. Everyday Health. Retrieved from https://www.everydayhealth.com/menopause/what-experts-want-bipoc-women-to-know-about-menopause/
- Yeager, S. (2024, February 1). Black women in menopause need better care. Feisty Menopause. Retrieved from https://www.feistymenopause.com/blog/Black-Women-in-Menopause-Care
- Wile Women. (n.d.). Do women of color experience perimenopause earlier? Retrieved from https://wilewomen.com/blogs/journal/do-women-of-color-experience-perimenopause-earlier
- Avis, N. E., Crawford, S. L., Greendale, G., Bromberger, J. T., Everson-Rose, S. A., Gold, E. B., Hess, R., Joffe, H., Kravitz, H. M., Tepper, P. G., & Thurston, R. C. (2015). Duration of Menopausal Vasomotor Symptoms Over the Menopause Transition. JAMA Internal Medicine, 175(4), 531-539. https://doi.org/10.1001/jamainternmed.2014.8063
- Harlow, S. D., Karvonen-Gutierrez, C. A., Jackson, E. A., & Thurston, R. C. (2022). Disparities in Reproductive Aging and Midlife Health Between Black and White Women: The Study of Women’s Health Across the Nation. Women’s Midlife Health, 8(1), Article 2. https://doi.org/10.1186/s40695-022-00073-y
- Ziv-Gal, A., Gallicchio, L., Whiteman, M. K., Visvanathan, K., & Manson, J. E. (2017). The Midlife Women’s Health Study: A Study Protocol of a Longitudinal Prospective Study on Predictors of Menopausal Hot Flashes. Women’s Midlife Health, 3, Article 2. https://doi.org/10.1186/s40695-017-0024-8
- Gupta, A. H. (2023, August 23). How Menopause Affects Women of Color. The New York Times. https://www.nytimes.com/2023/08/23/well/live/menopause-symptoms-women-of-color.html
- University of Michigan. (2023). 25 Years of Research Shows Insidious Effect of Racism on Black Women’s Menopausal Transition,Health. Michigan News. https://news.umich.edu/25-years-of-research-shows-insidious-effect-of-racism-on-black-womens-menopausal-transition-health/
MORE RELATED POSTS:










+leave a comment . . .